INTRODUCTION
Tobacco use kills nearly 1 in 2 long-term users with most deaths due to non-communicable diseases1. A 2014 epidemiologic study in California found that half of those who had been hospitalized for schizophrenia, bipolar disorder, or major depressive disorder, died due to diseases linked to tobacco use2. Cigarette smoking has been associated with depression, anxiety disorders, and schizophrenia3. Severe mental illnesses such as schizophrenia or bipolar disorder have been associated with a substantially reduced life expectancy compared to the general population. Much of this reduction is attributable to a 2–3 times greater risk of cardiovascular morbidity and mortality, an effect of tobacco use whose prevalence is up to 3.6 times greater among this population4.
People with mental illness are more likely to have stressful living conditions, have low annual household income, lack access to health insurance, healthcare, and help in quitting, which makes quitting more challenging5. Despite these barriers, motivation to quit smoking is high among individuals with mental illness and is comparable with estimates of intention to quit among the general population6. A 2014 meta-analysis of 26 tobacco intervention studies found that smoking cessation was significantly associated with decreased anxiety, depression and stress, and improvements in overall mood and quality of life7.
Kenya has the highest recorded smoking prevalence in Sub-Saharan Africa8, which is estimated at 12% of the adult population9. Five in ten smokers attempted to quit smoking in the past 12 months, and of those who attempted to quit, 7 in 10 smokers tried to quit without any assistance. Of the smokers who visited a healthcare provider in the past 12 months, only 3 in 10 were advised to quit smoking9.
The prevalence of mental disorders in Kenya is at 4%10, which is comparable with the prevalence rates of most high-income countries11. Although the burden of mental and neurological disorders in Kenya is high, diagnosis of these disorders is quite low. Ndetei et al.12, conducted a study in 10 general health facilities (excluding psychiatric wards) and found that 42% of inpatients and outpatients had symptoms of mild to severe depression. However, only 4% of patients had been diagnosed with a psychiatric condition12. The 2015 STEPS Survey-Kenya data reported an inconsistent association between tobacco use (both smoked and smokeless forms) and alcohol use (variable patterns)13-15. Studies by Lo et al.16 and Haregu et al.17 also evaluated this relationship, which demonstrated higher tobacco use prevalence rates among individuals who consume alcohol compared with those that do not. However, data from Lo et al.16 focused on an impoverished rural region, while data from Haregu et al.17 were limited to an urban slum population and explored only ‘unhealthy use of alcohol’ rather than moderate or low levels of alcohol use.
Research shows that the prevalence rates of tobacco use is higher among persons with mental health conditions, with greater nicotine dependence, greater withdrawal symptoms when quitting, and lower quit rates16,17. However, there are no cessation clinics in the primary psychiatric referral Mathari Teaching and Referral Hospital in Kenya, though the healthcare providers can provide brief support during consultations due to their training in mental health.
The current qualitative study was embedded in a controlled trial evaluating the effect of a group behavioral intervention on tobacco cessation among tobacco users with concomitant mental illness. In this report, we sought to identify the barriers and facilitators that participants faced in their cessation attempts during the study.
METHODS
Study design and setting
To gain more in-depth information on individuals’ experiences of cessation attempts, particularly barriers and facilitators while participating in a group behavioral tobacco cessation intervention (NCT04013724), a qualitative approach was chosen for data collection in this sub-study. This study was conducted at Mathari Referral and Teaching Hospital Clinic for Substance Abuse Treatment (CSAT) and outpatient follow-up clinics. Mathari Referral and Teaching Hospital is Kenya’s only national referral and teaching psychiatric hospital.
Study participants
Participants were selected from the intervention arm of the group behavioral intervention trial. Participants were aged ≥18 years, had a history of tobacco use for more than 6 months, were currently on outpatient follow-up treatment for a diagnosed mental health condition, and had consented to participate in the study for 6 months.
Study intervention
The group behavioral tobacco intervention consisted of 6 counseling sessions over 12 weeks, which were led by two trained facilitators, followed by monthly group meetings from weeks 14 to 26. The research team established rapport and empathy with the participants during facilitation of the group sessions. The program content was adapted from the Royal Australian College of General Practitioners’ Supporting Smoking Cessation Guide for Health Professionals and the World Health Organization’s Strengthening Health Systems for Treating Tobacco Dependence in Primary Care training package18,19.
The topics that were explored during the sessions included:
Introduction to the program and reasons to quit
Benefits of quitting and understanding why we smoke and ways of quitting
Withdrawal symptoms and social support
Dealing with stress and anxiety and coping with depression due to withdrawal
Assertiveness training and anger management
Tobacco-free lifestyle and dealing with high risk situations
Focus groups’ questions were related to participants’ overall experience with their quit attempts, nicotine withdrawal, other barriers, and facilitators that they perceived to be effective, particularly those strategies that were not explicitly part of the study’s intervention.
The study team primarily used the local language (Kiswahili) to ask questions, and ‘Sheng’ (local dialect) to probe deeper or clarify the participants’ comments. The principal investigator (YO) used a prepared set of questions to guide the group discussions (Supplementary file). Sessions lasted approximately 45 minutes. Process field notes were used to record the group discussions by YO and a trained research assistant (completing a Master’s degree in counselling psychology) in fundamental research methods. Field notes were chosen as the mode of data collection because some participants were not comfortable with video or audio recording. Field notes documented discussions as accurately as possible during and after group discussions. Participants were no longer recruited for group discussions when saturation of themes had been reached. Participants were not invited to check the transcriptions, and thus, no respondent validation was undertaken.
Participants were offered 200 Kenya shillings (about US$2) for the time taken to participate in the group discussions. Ethical approval was obtained from Kenyatta National Hospital/Nairobi University Ethical Review Committee (ERC). All participants provided informed consent.
Data collection
A purposive sample of 49 tobacco-using patients with concomitant mental illness was drawn from 5 intervention groups (10 participants per group, and one group had one participant withdraw from the study due to severe withdrawals at the beginning of the study) of the larger controlled trial whose methods have been published20. Data collection took place between March 2017 and August 2019. Focus group discussions were held bimonthly for the first 3 months and monthly for the next 3 months, before the start of the group behavioral tobacco cessation counseling sessions. Questions focused on their experiences with practicing what they had learnt in their previous group therapy session. Group discussions were facilitated by YO who has experience in facilitating group discussions and who was involved in the delivery of the trial. In addition to field notes to capture group discussions, characteristics of study participants, such as age, sex, residence, education level, occupation, and perceived health status, were recorded.
Data analysis
Quantitative data were summarized and were reported as proportions for categorical variables and means with standard deviations, or medians with interquartile ranges if data were skewed. Qualitative data were analyzed using an inductive approach, allowing identification of emerging themes from the data. The research team focused firstly on individual group transcripts before seeking common themes across all the groups’ data. Handwritten notes were transcribed into electronic format (Microsoft Word initially and subsequently transferred to Microsoft Excel; 1 comment per spreadsheet cell) by YO and checked by another member of the study team (analyst triangulation ).
Comments from each group were cross-referenced and compared, ensuring all comments were recorded accurately while duplicate entries were removed. A final list of focused comments was compiled for analysis. Themes were identified and color coded on the spreadsheet. Microsoft Excel’s filter was used to sort cells by color to identify thematic areas. A second pass of data identified overlapping comments and led to consolidation of some codes. Codes applied were keywords to categorize or organize text into themes by YO, and data were analyzed in accordance with the process described by Braun and Clarke21. The next stage involved interpreting the data by identifying any recurring themes throughout and by highlighting similarities and differences in the data across groups. The final stage involved data verification, which involved rechecking the field notes and codes.
RESULTS
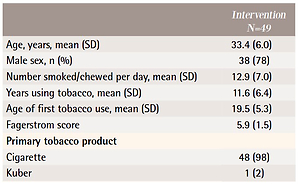
Table 1 outlines participants’ baseline characteristics. Mean (SD) age of participants was 33.4 (6) years, and most (78%) were male. Nearly half (45%) were unemployed. Most participants (80%) had substance use disorders, while more than 2 in 3 (70%) were using other drugs (substance use). Major depression was reported by 10%, 4% reported schizophrenia and a similar number reported bipolar mood disorder. Almost all participants (98%) were using cigarettes.
Table 1
Baseline sociodemographic and clinical characteristics of the study participants (N=49)
Qualitative findings
Barriers for quitting tobacco use
1. Peer influence and support
Most participants were smoking in groups, including after the group sessions or while they were working together, or ‘hustling’ together.
‘Me, I would like to quit but after the session, when walking to the bus stop, we walk as a group and when others are smoking, I just have to. The smell of the cigarette is in your face, you just have to.’ (34-year-old, female)
‘When with others you don't have to worry about smoking, it is free, everyone just gives you a puff.’ (35-year-old, male)
‘I just have to smoke when with my friends, they are the ones who support me when am stuck. If I avoid them because I have stopped smoking, what will I do when I get stuck and I don't have other friends? They might also think [I] am the one reporting what we do. Maybe later, not now.’ (29-year-old, male)
2. Withdrawal symptoms
Most participants reported feeling nausea, dizziness, headaches, depressed, cravings, insomnia, coughing, moodiness and numbness associated with withdrawal, which made quitting challenging.
‘In the morning, I have a serious headache that I cannot even walk. Then I feel like fainting…at such a time I have to smoke so that I feel normal. Otherwise I cannot do anything.’ (45-year-old, male)
3. Fear of complete cessation
Most participants had problems with quitting completely, and faced strongest urges associated with the first morning and last evening cigarettes. Others did not want to be completely drug-free, so they continued to smoke because it carried relatively lower risks compared with other drugs in terms of their daily functioning.
‘Madam, I have worked on reducing smoking. I have given up alcohol and heroin. At least I need something small to keep me high.’ (23-year-old, male)
4. Other substance use
Most participants reported using other substances that increased their cravings. These included alcohol, methadone, bhang, and khat. Those who were using methadone reported intense cravings, especially after their daily dose of methadone. Others reported having started smoking cigarettes after initiation to the methadone program. They also had a ‘base’ where they used to meet within the hospital just after their methadone doses and would share their cigarettes.
‘Madam, the taste of methadone is very bitter, only the taste of cigarettes takes it away. During the day [I] am able to stay without smoking, but after taking methadone, I have to take a smoke to clear the bad taste.’ (20-year-old, female)
‘Because I remember the effects of cigarettes smoking that you mentioned, it is better to smoke bhang… as I have to smoke something. It calms me down.’ (35-year-old, male)
5. End-of-month disputes
Most participants reported experiencing family disputes, housing problems, or problems with landlords that were exacerbated at the end of each month. During the sessions, it was noted that most participants increased the number of cigarettes smoked at the end of the month. This theme was explored, and most participants reported fears of not affording their house rents and delayed payments as a serious trigger.
‘It is easier to worry when you are puffing at something.’ (32-year-old, female)
6. Boredom
Some participants reported that they smoked more when they were idle or felt bored. But when participants were busy, they had no time to smoke
‘When I have no work and [I] am just relaxing, or bored, smoking keeps me busy.’ (31-year-old, male)
Facilitators to supplement cessation attempts
Since the study did not provide nicotine replacement therapy (NRT) to participants to assist in combating their cravings, withdrawals, and sustainment of their cessation attempts, some participants added their own facilitators to supplement the study’s group behavioral counseling strategies. Themes included:
1. Oral stimulation
Most participants reported that as long as their mouths were busy, then they did not have cravings. Strategies used included: eating raw eggs, sweets and bananas, and chewing gum. Some participants reported that raw eggs alleviated feelings of withdrawals and managed headaches. Some participants realized that chewing gum or eating tropical (e.g. mint flavored) sweets delayed cravings for smoking.
‘My father stopped smoking by swallowing 2 raw eggs in the morning. When I started my quit attempt, and was struggling, I thought to try his way. The first day it was difficult, but after a while I got used to it, and I realized I had reduced my smoking drastically. So, I shared with some of our group members.’ (26-year-old, male )
‘The cigarettes I smoke have menthol, and the tropical sweets or chewing gum give me a similar taste, and I believe confuses my mind that [I] am smoking.’ (40-year-old, female )
2. Spousal and friend support
Participants reported sharing what they were learning during the intervention sessions with their spouses, families, and friends. Strategies included: throwing away cigarettes and lighters found in the house, not smoking in the home, and not being allowed to smoke in the presence of family and friends. Some participants made a pact with their spouses to throw away any of their cigarettes if they found them. Unfortunately, all participants who tried this strategy relapsed, including trying to smoke cigarettes that were wet.
‘My wife would wait for me to come home and change, search through my clothes and throw away the cigarettes in water. First day she searched the whole house and threw away all of my cigarettes.’ (39-yearold, male)
Some participants decided to stop sharing their cigarettes with friends and to stop borrowing cigarettes. This helped them smoke only the cigarettes that they had bought, and most participants reported buying single sticks to aid in reduction of amounts.
‘I only buy one cigarette and smoke it in bits throughout the day. I have stopped taking puffs from others, and I also don't give puffs. I therefore smoke less amounts.’ (28-year-old, female)
A sub-theme included cutting down, whereas some participants reported fear of quitting without medication due to their previous quit attempts.
‘I don't think just stopping completely will be possible for me. Since the program is for some months, I will focus on reducing at least 2 sticks every week until I stop completely.’ (33-year-old, female)
Additional observations
First, two groups started their own ‘table banking’ groups with the transport token they used to receive during their session days. Table banking is groupbased funding strategy in which members save and borrow immediately during their meeting times to ensure all group members attended the counseling sessions so that each can receive his/her token for their contribution. With this initiative, other patients who had not been part of the study started requesting to be part of the study. These two groups thus worked to spread news that there were cessation sessions available at the hospital.
Second, during the group discussions, participants reported that they would have preferred more frequent group behavioral intervention sessions than the biweekly meetings, and as such, they created WhatsApp or short message service groups. According to these participants, the idea that they were going to be asked about their tobacco use experiences made them work harder at quitting attempts. Group meetings also encouraged them to continue making quit attempts, because the participants perceived that they were competing to see who was making the most progress.
Third, participants in the different groups started checking on each other and working as informal support groups. They formed a WhatsApp group that they used to remind each other of the meeting dates. Unfortunately, some participants were unable to afford internet and could not participate in the group. This led to reduction of the group interactions, but enhanced short message communication, which was cheaper. Some participants used their parents’/spouses’ phones as they did not have their own, and some parents/ spouses began calling to check if the participants had attended the group meetings. If a participant was late in attending, or missed a session, then they would call each other. When two members became pregnant while in the study, they kept reminding each other of the impact of tobacco use on the fetus.
Fourth, participants highlighted the need for more regular interactions. Support groups to complement group therapy sessions could be considered when integrating tobacco cessation programs and these warrant further study. Participants’ competitiveness could also be addressed to ensure continuous attempts, as those who were not making rapid progress felt discouraged.
DISCUSSION
Summary of results
The study identified barriers experienced by study participants in their quit attempts, including: 1) peer-influence, 2) withdrawal symptoms, 3) fear of complete cessation, 4) other substance use, 5) end-of-month disputes, and 6) boredom. To manage the above barriers, participants variably incorporated facilitators that were not part of the group behavioral sessions, including: 1) oral stimulation, and 2) spousal and friend support.
To our knowledge, this is the first study reporting on the barriers and facilitators in cessation attempts for tobacco users with concomitant mental illness attending group tobacco cessation therapy in Nairobi, Kenya. Smoking cessation interventions are among the most cost-effective interventions available in reducing the risk of mortality among tobacco users22. Group therapy has been shown to offer the added value of fostering peer support and is likely to be more cost-effective than individual counseling. Group cognitive behavioral therapy programs of approximately 8–10 individuals that meet weekly for 7–10 weeks have been shown to have the most successful quit rates for the mental health vulnerable population, compared to individual counselling23.
Results in context
The current study highlighted that most barriers faced by people who have mental illness and use tobacco are similar to those faced by the general population24. Participants in the current study were worried about withdrawal symptoms, particularly headaches and cravings. Participants expressed greatest concern about not being able to concentrate, and therefore, being tobacco-free was perceived as potentially counterproductive for them. Introduction to the benefits of tobacco cessation pharmacotherapies in management of nicotine withdrawal symptoms would be important to participants who find it difficult to manage withdrawal symptoms with behavioral coping skills only.
Some were concerned about losing friends. Most worried that since they had already used tobacco for years, its effects were irreversible, and so continuing to smoke would not likely change their long-term health. To address the fears of tobacco effects’ irreversibility as mentioned by some participants, populations suffering mental health conditions can be taught about health and quality of life gains in quitting, even later in life.
Some participants did not want to quit because they felt it made them feel better and improved their symptoms, especially those associated with depression. Most participants who were worried about alleviating their psychotic symptoms reported wanting to reduce smoking, but not to quit completely. Participants who did not want to quit completely can be offered tailored cessation interventions that address their psychotic symptoms or alternatives for alleviating them that do not involve tobacco use.
Most barriers experienced by the participants have been reported among the general population but some facilitators, like swallowing raw eggs, were less common. This could have been borrowed from some of the practices used by alcohol consumers where raw eggs have been marketed to treat alcohol-related hangovers25. Peer pressure as a barrier was expected, because it is commonly experienced among tobacco users attempting cessation24. This population that was meeting regularly for their psychiatric follow-up may have been more susceptible to peer pressure, but this is speculative. The importance of assertiveness and assertiveness training should be included in future cessation programs.
Prevalence of other substance use among this population has been documented, and is a reported barrier to tobacco cessation26 because many people with mental illness use other substances to block their psychotic episodes, increase their mood, or give them a euphoric effect particularly when feeling depressed27. There is a need to include practical management skills for other substances of abuse.
Similar to the current study results, Twyman et al.24 noted that barriers to quitting smoking, endorsed by numerous studies, included smoking for stress management, boredom, social acceptability of smoking, lack of support to quit, and lack of access to resources to quit. Findings in the current study showed that participants complained that one of the barriers they experienced was boredom. This has been shown to be similar with the general population24. Time management should be included in a cessation program, to assist with management of boredom, as half of the participants were unemployed.
Smoking to reduce stress was a frequently reported barrier, particularly towards the end of the month and largely due to financial constraints. Studies have shown that smokers typically demonstrate higher levels of stress and low mood state than non-smokers and ex-smokers. Unemployment, financial stress, and poverty, which are stressors associated with vulnerable groups, may compound stress levels28. Group behavioral tobacco cessation could offer more intensive stress management sessions, as well as offer skills for setting up small-scale businesses (income generating activities) on their own that do not require large amounts of capital to set up.
It is believed that the focus groups enabled the participants to share their experiences openly; and in the process, they were able to challenge as well as encourage each other on alternatives that have worked or not worked in the process of their cessation attempts. This sharing is presumed to have led to change in tobacco use patterns (successful quits and reduction in use). According to Prochaska et al.29, when information is availed, a person can move from one stage of change to the other. Even when someone experiences a relapse, he will not revert to pre-contemplation, but will always seek a way to move to the next stage29.
Based on these results, the current study identifies the need to address barriers by improving the acceptability, accessibility, and perceived appropriateness of cessation interventions to tobacco users with concomitant mental illness by contextualizing and adapting evidence-based interventions. Contextualization needs to be incorporated into policies that seek to ensure that cessation interventions meet the needs of their intended populations.
Strengths and limitations
The study has several strengths. First, it was conducted in the participants’ usual environments, as well as during outpatient clinic follow-up days, which signals that this group can be naturally implemented. Second, the study focused on strategies that were readily available and did not have significant direct costs for participants in terms of attending group therapy. Third, the study was performed in a novel setting in a high-risk vulnerable group of tobacco users with concomitant mental illness, highlighting the clinical significance of the intervention. However, this study also has several limitations. First, we used field notes rather than audio recording to capture data based on participants’ preferences. While it may be possible that additional information or findings could have been derived from transcriptions of audio recordings, this method of data capture was necessary to respect participants’ autonomy. It is likely that we captured major themes from discussions using the study methods, which may have led to more open discussions than may not have been possible with audio recording. Second, the generalizability of the study is limited because it recruited participants who were part of a larger intervention trial at a single referral center, and the sample size was also small. Third, we were not able to directly compare the study findings to other populations, including the control group, from whom we did not seek similar information. However, we sought to perform triangulation during data collection and analysis to improve the rigor and reliability of the study findings. Fourth, a limitation with the qualitative analysis was that participants were not invited to check the transcriptions, and thus, no respondent validation was undertaken.
CONCLUSIONS
Achieving successful tobacco cessation intervention can be challenging among individuals with concomitant mental illness, particularly when nicotine replacement therapy and other pharmacotherapies to manage symptoms of withdrawal are neither available nor affordable. However, this study provides insights into key barriers and facilitators to tobacco cessation in this population in the context of a group behavioral counseling intervention trial. Areas of further study include: 1) provision of quit/non-smoking groups to offer virtual or face-to-face peer support for those who are making quit attempts; 2) evaluating the effect of a greater dose of group tobacco behavioral counseling since most participants requested for more regular interactions; and 3) supplementing group behavioral sessions with virtual or telephonic follow-up by healthcare professionals. New strategies are urgently needed to be contextualized, implemented and evaluated to help reduce the substantial burden of disease that this vulnerable population faces.