INTRODUCTION
The use of tobacco has changed dramatically over the past several years. While cigarette smoking has fallen to historic lows among US adults1, there has been a marked increase in the use of electronic nicotine delivery systems (ENDS), and approximately 4.6% of adults are current users2. In cases of dual use (both cigarettes and ENDS), recent research indicates that many dual users progress to exclusively using cigarettes3. Historically, lesbian, gay and bisexual (LGB) individuals have higher rates of smoking4, often attributed to targeted tobacco advertising5,6, exposure to stressors (i.e. minority status, stigma, homophobia, and gay bashing)7,8 and psychological distress9. The same tendency of elevated ENDS use among LGB individuals has recently been documented10. However, LGB groups are not homogeneous and differences may exist between tobacco use by men and women within the groups.
Compared to heterosexual women, current cigarette use (past 30 days) has been found to be consistently higher among lesbian and bisexual women11–16. A similar finding for current cigarette use was noted when comparing gay and heterosexual men11–16, but elevated use among bisexual men has not been a consistent finding12–15.
Despite rapid proliferation of ENDS use, few studies have examined use of such devices by LGB individuals and, when investigations have occurred, the findings are less consistent than findings for cigarette smoking10,11,15,16. Current ENDS use has been found to be higher in bisexual women11,15 compared to heterosexual women, and in bisexual men16 compared to heterosexual men. No differences have been observed when comparing lesbian women and gay men to their heterosexual counterparts. One national survey found higher rates of dual cigarette and ENDS use among LGB adults, but that difference was not significant17. The purpose of this research was to examine differences in cigarette smoking, ENDS use and dual use among LGB subgroups.
METHODS
Sample
The study sample comprised 2087 individuals (918 men, 1169 women) from a national survey of adults (aged ≥18 years) who were current ENDS users and/or current cigarette smokers. Recruitment took place from 24 June to 11 August 2016 and, on behalf of the American Heart Association Tobacco Regulation and Addiction Center (A-TRAC), was conducted by Research Now and Survey Sampling International (SSI), a marketing research vendor, via their online panels and those of their partners. Approximately 13000 individuals received emails inviting them to complete the online survey, with a targeted 20% response rate. A quota sampling method was employed to ensure diversity (e.g. age, gender, race/ethnicity, sexual orientation) and the ability to compare across groups; thus, the final sample was not intended to be representative of the US population. The Institutional Review Board of the University of Mississippi Medical Center approved the study.
Once participants gave consent, they responded to a questionnaire about selected sociodemographic and economic characteristics and items about their knowledge of, attitudes toward, perceptions of, and behavior regarding an array of tobacco products, including ENDS. Participants remained anonymous, as no personal identifying information was collected.
Measures
We examined the relationship between sexual orientation and current tobacco product use, including ENDS, cigarettes, and dual use. Current ENDS users were participants who used an ENDS device within the past 30 days and had used it for 3 months or more, which is consistent with the Population Assessment of Tobacco and Health Study and other studies18–20. Current cigarette smokers were those who smoked cigarettes in the past 30 days and smoked 100 or more cigarettes in their lifetime. Current dual users were participants who currently used both ENDS and cigarettes. Participant characteristics included demographics (age, sex, race, ethnicity) and socioeconomic status (education, income, employment status), marital status, and sexual orientation.
Statistical analysis
Descriptive characteristics were expressed as frequency (%) for all participants. Differences in the characteristics across heterosexual, lesbian, gay and bisexual participants were assessed using chi-square test. The relationship between sexual orientation and multiple tobacco use status (dual use, ENDS use only, cigarette smoking only) was examined using multinomial logistic regression21, with adjustment for age, race, ethnicity, education, income, employment status, and marital status. The adjusted odds ratio (AOR) for tobacco-product use (with cigarette smoking only as the reference outcome) and corresponding 95% confidence intervals (CI) are reported. Separate analyses were conducted for male and female participants because men and women used tobacco products disproportionally and our objective was to evaluate the association of sexual orientation with tobacco use. A two-sided p-value <0.05 was considered statistically significant. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
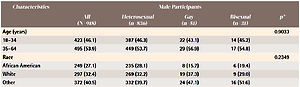
Of the 2087 participants, gay/lesbian and bisexual participants accounted for approximately 9% of male and 19% of female participants (Table 1). Male participants were similar in age, race, education, income, and employment status across gays, bisexuals and heterosexuals. However, ethnic representation and marital status varied significantly by sexual orientation (Table 1, Males). Specifically, 74.2% of bisexual men were Hispanic compared to 50.8% of heterosexuals and 54.9% of gay men, and 76.5% of gay men and 74.2% of bisexual men were not married compared to 53.8% of heterosexuals. In contrast, female participants significantly differed between lesbians, bisexuals and heterosexuals for almost all the characteristics except employment status (Table 1, Females). For example, lesbian and bisexual women were younger and more likely to be Hispanic, unmarried, and earn less income.
Table 1
Characteristics of current ENDS users and/or current cigarette smokers
| Characteristics | Male Participants | ||||
|---|---|---|---|---|---|
| All (N=918) | Heterosexual (n=836) | Gay (n=51) | Bisexual (n=31) | Gay (n=51) | |
| Age (years) | 0.9033 | ||||
| 18–34 | 423 (46.1) | 387 (46.3) | 22 (43.1) | 14 (45.2) | |
| 35–64 | 495 (53.9) | 449 (53.7) | 29 (56.9) | 17 (54.8) | |
| Race | 0.2349 | ||||
| African American | 249 (27.1) | 235 (28.1) | 8 (15.7) | 6 (19.4) | |
| White | 297 (32.4) | 269 (32.2) | 19 (37.3) | 9 (29.0) | |
| Other | 372 (40.5) | 332 (39.7) | 24 (47.1) | 16 (51.6) | |
| Ethnicity | 0.0345 | ||||
| Hispanic | 476 (51.9) | 425 (50.8) | 28 (54.9) | 23 (74.2) | |
| Non-Hispanic | 442 (48.1) | 411 (49.2) | 23 (45.1) | 8 (25.8) | |
| Education | 0.3246 | ||||
| HS or lower | 254 (27.7) | 237 (28.3) | 10 (19.6) | 7 (22.6) | |
| Above HS | 664 (72.3) | 599 (71.7) | 41 (80.4) | 24 (77.4) | |
| Income (US$) | 0.9470 | ||||
| <50000 | 362 (39.4) | 332 (39.7) | 19 (37.3) | 11 (35.5) | |
| 50000–89999 | 342 (37.3) | 311 (37.2) | 20 (39.2) | 11 (35.5) | |
| ≥90000 | 214 (23.3) | 193 (23.1) | 12 (23.5) | 9 (29.0) | |
| Employment status | 0.4780 | ||||
| Employed | 716 (78.0) | 650 (77.8) | 43 (84.3) | 23 (74.2) | |
| Unemployed | 202 (22.0) | 186 (22.2) | 8 (15.7) | 8 (25.8) | |
| Marital status | 0.0007 | ||||
| Married | 406 (44.2) | 386 (46.2) | 12 (23.5) | 8 (25.8) | |
| Not married | 512 (55.8) | 450 (53.8) | 39 (76.5) | 23 (74.2) | |
| Tobacco-use status | 0.8618 | ||||
| Current smokers only | 212 (23.1) | 190 (22.7) | 14 (27.5) | 8 (25.8) | |
| Current ENDS users only | 417 (45.4) | 380 (45.5) | 24 (47.1) | 13 (41.9) | |
| Current dual users | 289 (31.5) | 266 (31.8) | 13 (25.5) | 10 (32.3) | |
| Characteristics | Female Participants | ||||
| All (N=1169) | Heterosexual (n=945) | Lesbian (n=62) | Bisexual (n=162) | p* | |
| Age (years) | <0.0001 | ||||
| 18–34 | 660 (56.5) | 496 (52.5) | 36 (58.1) | 128 (79.0) | |
| 35–64 | 509 (43.5) | 449 (47.5) | 26 (41.9) | 34 (21.0) | |
| Race | <0.0001 | ||||
| African American | 372 (31.8) | 309 (32.7) | 20 (32.3) | 43 (26.5) | |
| White | 363 (31.1) | 321 (34.0) | 11 (17.7) | 31 (19.1) | |
| Other | 434 (37.1) | 315 (33.3) | 31 (50.0) | 88 (54.3) | |
| Ethnicity | <0.0001 | ||||
| Hispanic | 575 (49.2) | 424 (44.9) | 42 (67.7) | 109 (67.3) | |
| Non-Hispanic | 594 (50.8) | 521 (55.1) | 20 (32.3) | 53 (32.7) | |
| Education | 0.0141 | ||||
| HS or lower | 343 (29.3) | 261 (27.6) | 19 (30.6) | 63 (38.9) | |
| Above HS | 826 (70.7) | 684 (72.4) | 43 (69.4) | 99 (61.1) | |
| Income (US$) | 0.0109 | ||||
| <50000 | 622 (53.2) | 494 (52.3) | 25 (40.3) | 103 (63.6) | |
| 50000–89999 | 373 (31.9) | 303 (32.1) | 25 (40.3) | 45 (27.8) | |
| ≥90000 | 174 (14.9) | 148 (15.7) | 12 (19.4) | 14 (8.6) | |
| Employment status | 0.4063 | ||||
| Employed | 775 (66.3) | 634 (67.1) | 37 (59.7) | 104 (64.2) | |
| Unemployed | 394 (33.7) | 311 (32.9) | 25 (40.3) | 58 (35.8) | |
| Marital status | <0.0001 | ||||
| Married | 373 (31.9) | 333 (35.2) | 9 (14.5) | 31 (19.1) | |
| Not married | 796 (68.1) | 612 (64.8) | 53 (85.5) | 131 (80.9) | |
| Tobacco-use status | 0.0569 | ||||
| Current smokers only | 425 (36.4) | 358 (37.9) | 23 (37.1) | 44 (27.2) | |
| Current ENDS users only | 379 (32.4) | 306 (32.4) | 20 (32.3) | 53 (32.7) | |
| Current dual users | 365 (31.2) | 281 (29.7) | 19 (30.6) | 65 (40.1) | |
For multiple tobacco use status, after adjusting for demographics, socioeconomic status, and marital status, there were no significant differences in the likelihood of current ENDS use only or dual use as opposed to cigarette smoking only between gay men and their heterosexual counterparts, or between bisexual men and their heterosexual counterparts (Table 2, Males). However, bisexual women were 1.85 times (AOR=1.85; 95% CI: 1.19–2.87; p=0.0062) more likely to report dual use in contrast to cigarette only use compared to heterosexual women, but there was no difference in the likelihood of current ENDS only use as opposed to cigarette smoking only between bisexual and heterosexual women (Table 2, Females). Also, no significant differences were found in the likelihood of tobacco use between lesbian and heterosexual women.
Table 2
Likelihood of current dual use (vs cigarette only use) and current ENDS use only relative to cigarette smoking, by sexual orientation, separately for male and female participants
[i] Adjusted odds ratios (AOR) and 95% confidence intervals (CI) of lesbian/gay and bisexual participants were estimated from multinomial logistic regression for multiple tobacco use response (current dual use and current ENDS use only as opposed to current cigarette smoking only). Separate analyses were performed for male and female participants, with adjustment for age, race, ethnicity, education, income, employment status, and marital status.
DISCUSSION
Similar to the findings of Li et al.15 and Emory et al.11, our findings support that there is increased current use of ENDS among bisexual women compared to heterosexual or lesbian women when controlling for demographic variables. While Li et al.15 focused on participants aged 18–25 years, the age of our participants was similar to those of Emory et al.11 in that we recruited participants up to 64 years old. In contrast, Hoffman et al.16 found no difference in ‘current’ ENDS use and an increase in ‘ever’ ENDS use among bisexual women. When examining ENDS use in terms of ‘lifetime’ use, Wheldon et al.22 found lesbian and bisexual women were at greater risk compared to heterosexual women. One important finding from our study is the increased risk of dual use (ENDS and cigarettes) among bisexual women. When examining poly-tobacco use, Delahanty et al.23 found bisexual women were more likely to use two or more tobacco products compared to gay men. However, within the LGB groups, differences in the use of combustible plus non-combustible products were not found. As additional investigations take place, it is important to clarify product-use behaviors (e.g. various combinations for dual use or poly-use, frequency and intensity of use, type and contents) to more fully understand harm potential.
The findings in this study regarding men were similar to those of both Li et al.15 and Emory et al.11 in that there was no difference in current ENDS use when comparing gay or bisexual men to their heterosexual counterparts. In contrast, Hoffman et al.16 found a difference when comparing male bisexual ever ENDS use and current ENDS use to their heterosexual counterparts16. It is important to note that their sample contained greater than 3000 gay/bisexual men, which may have allowed for greater sensitivity to detect ENDS use differences.
Strengths and limitations
A strength of our study was the large national sample of tobacco users allowing us to stratify by sex and sexual orientation. In addition, the sex-stratified analysis of LGB participants permitted a more precise view of ENDS behaviors. Despite its strengths, our study has a number of limitations. First, the sample was not representative of the US population, limiting the nature of potential analyses. Second, the data are cross-sectional; thus, we are not able to assess any changes over time. In addition, as with all survey studies, there is a risk of recall and self-report biases, and participation required internet access. Nevertheless, our findings contribute to the literature on tobacco product use by LGB groups. While we conducted separate analyses on LGB men and women, future research exploring tobacco use with the interaction of sexual orientation and sex may provide useful insights.
CONCLUSIONS
When controlling for demographic factors, there is increased likelihood of dual use, among bisexual women compared to lesbian or heterosexual women. This report is one of the first to reveal significantly elevated patterns of dual use in this group, a finding that should be further addressed in future research. These findings, especially the greater use patterns by bisexual women, suggest that targeted health messages may be needed to raise awareness of risk in specific LGB groups and that future research with these populations is necessary to better understand differences in tobacco perceptions and use.