INTRODUCTION
One in four US high-school students currently use some form of tobacco, with 9.3 % of these tobacco users reporting smoking combustible cigarettes in the past 30 days in 20151. The onset of smoking before the age of 18 years hastens nicotine dependence, elevating risks for detrimental and lasting effects on the developing brain and sustained tobacco use2. Although the percentage of US adolescents reporting combustible cigarette use is at a historic low1, with all products combined (e.g. cigars, e-cigarettes, smokeless tobacco), the overall tobacco use prevalence remains unchanged over the past two decades1-5. Even though over half of current adolescent smokers express a desire to quit, most who seek cessation treatment face numerous challenges and ultimately fail6-8.
Despite considerable research on predictors of adolescent tobacco cessation, tobacco control experts continue to grapple with low cessation rates. Youth tobacco cessation rates range between 7-12 %9,10. Adolescent cessation studies conventionally de-emphasize failed treatment rates among cessation seekers, favoring instead to report the predictors of successful cessation outcomes or not reporting outcomes other than complete abstinence. Given the typical focus on individual-level data, underscoring failed outcomes may be perceived as pointing to something innately wrong or lacking with the individual adolescent’s capacity to quit. An alternative and novel view, as proposed in this study, is the examination of ‘failure’ not as failure of the individual adolescent but a failure of the treatment and the treatment environment to meet individual needs or risks. Moreover, while the understanding of individual-level factors related to both successful and failed treatment is important, examination of the interplay of factors beyond the individual that affect treatment outcomes is critical. It is plausible, for instance, that socio-economic factors or a combination of factors, including the occupations, education levels, income and wealth within localities proximal to adolescents may partially explain tobacco use. Research increasingly demonstrates that tobacco use is influenced by a myriad of socio-environmental factors. For instance, studies show notable variation of smoking prevalence rates across schools, regardless of individual-level factors11-13, suggesting direct pathways between schools and adolescent tobacco use, tobacco attitudes, and motivation to quit tobacco14-16. School-level determinants are known to explain between 4% to 40% of the variation in smoking, across both middle and high-school aged students11. Many studies also demonstrate that smoking in adulthood is influenced by childhood socio-economic disadvantage17-19.
Acknowledging tobacco control as a complex and dynamic system, there have been numerous calls, from policy makers and the research community, to consider a systems perspective that expounds the complex socio-environmental influences of tobacco use20,21. Behavioral theories, such as Bronfenbrenner’s Ecological Systems theory22, emphasize the role of socio-environmental factors beyond the individual that influence health behaviors. Tobacco users are influenced not only by demographic, biological and psychological factors, but also by external forces such as governments, industries and social environments, including schools, neighborhoods and workplaces. Forces within these environments5,20 may influence tobacco use behaviors through macro-scaled strategies, including State tobacco control funding or taxation, tobacco industry marketing, and State or county clean-indoor air regulations3,23-28. While conceptual thinking touts the benefits of multilevel synergistic tobacco control initiatives, practical implementation has been slow, in part because the requisite research has not been conducted. The lack of empirical literature describing the application of comprehensive models that capture and account for multi-level influences has impeded real-world application and results. While there is some research showing that adult smoking cessation treatment can be moderated by these strategies29, the field knows very little about the relative contribution of these factors on adolescent tobacco cessation. To bridge this literature gap, the present article describes an innovative socio-spatial approach to measure and explain the multi-level socio-environmental influences on adolescent tobacco cessation. By exploring the contributions of socio-environmental risk among adolescents who experience failed treatment it is possible to glean guidance in reducing cessation program failure, especially for adolescents who generally need it the most.
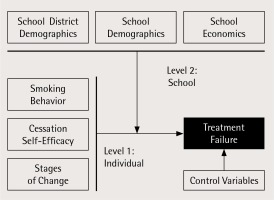
The study goal was to explain how person- and place-based social factors can influence smoking cessation outcomes among adolescents enrolled in a cessation treatment program spanning over a decade in many States. The present research adapted a multilevel socio-ecological model (Figure 1) to examine more specifically the influence of school-level socio-environmental factors, including school-level demographics and economics, on adolescent smoking cessation failure20. Analyses also examined the extent to which the school environment moderated the relationship between individual-level predictors (e.g. cessation self-efficacy and number of cigarettes per day) and cessation failure. Secondary data capitalized on various existing sources, including a longitudinal-data set obtained from studies of a national school-based adolescent smoking cessation program (American Lung Association’s Not-On-Tobacco, N-O-T)30-33. The environment of focus is the school, as N-O-T delivery historically occurs in schools. Schools are well established important settings for health promotion, including smoking cessation and offering a sustained and effective avenue for reaching the adolescent population.
METHODS
Data sources
By linking individual data to geo-referenced school-level data, researchers established a tobacco-specific socio-spatial evaluation allowing active consideration of space, place, personal and social indicators on smoking cessation. For the present research aim, two levels of data were used to fulfil our evaluation: individual-level data (Level 1) from adolescent cigarette smokers, and school-level data (Level 2) linked to those individuals through geo-referenced codes. Data on individual-level adolescent smokers (N=8855) came from de-identified aggregated original sources from 28 separate evaluation trials31 from 5 States spanning 1997-2012. Table 1 summarizes the variables in the individual-level and school-level data. Enrolled adolescents sought treatment voluntarily and were enrolled in either brief or intensive treatments (i.e. 10-15 minute one-time advice to quit vs N-O-T), both treatments had the goal of smoking cessation. In all trials, participants were current smokers (≥1 cigarettes per day or CPD, in past 30 days) and between 14-19 years old. Similar methodology was used across studies including design, instrumentation, recruitment, and data collection procedures. Refer to previously published trials for details31,34,35. The present study received Institutional Review Board (IRB) approval for exemption (45 CFR 46.101, b. 1).
Table 1
Key study variables
It is important to point out that while the individual level cessation trials had an initial goal to evaluate the efficacy of the N-O-T program, the present investigation sought to understand treatment failure among cessation seeking adolescents, regardless of treatment type. Thus, treatment conditions are not compared in the present investigation. However, statistical analyses controlled for treatment group to account for a known source of variation in outcomes in all models. For the present investigation, treatment failure is operationally defined as not achieving the primary goal of smoking cessation among all participants, measured 3-months post baseline.
School-level data were associated with the schools that participated in the adolescent smoking cessation trials in five States: FL, NC, WV, WI and NJ. Each school was uniquely geo-referenced by postal ZIP code, a National Center for Education Statistics-Identification Number (NCES-ID), and a Federal Information Processing Standard code (FIPS). The NCES, a part of the US Department of Education, is charged with collecting, collating and analyzing data on the education systems and schools. The NCES maintains a publicly available database of school and school-district data. The study used the NCES-ID to gather school-specific data including enrollment, number of full-time teachers, student-teacher ratio, and students eligible for free or reduced lunch from the NCES database. FIPS codes provided access to the publicly available US Census Bureau database to gather school-district level data for each school, including education level of individuals within the district, employment levels, and percentage of the district population living in poverty. A separate database was constructed containing all school-level data. The final step was to form a relational sociospatial database that connected all separate databases: 1) individual-level data containing information on each participant in the adolescent smoking cessation trials—this database included the geo-referenced code indicating the participant’s school where the cessation program was conducted; and 2) school-level data containing both NCES and US Census Bureau information.
Measures
Outcome variables
Treatment failure. Using the intent-to-treat (ITT) sample, participants were considered to have experienced failure to quit if they reported continuing smoking or were not available for follow-up at 3-months post baseline. Conservatively, analysis assumed that unavailable participants continued to smoke, accounting for 27% of the treatment failure sample34,36. The study uniquely applied ‘treatment failure’, unlike the majority of tobacco cessation studies that commonly focus on quit rates9,37-39. Such an approach was intended to uncover important previously unknown information on the reasons why cessation treatments failed with adolescents who are regarded most at risk.
Predictor variables
The study included predictor variables that are well established in previous trials of the team and in other existing tobacco control literature34,35. Specifically, the model included factors associated with adolescent tobacco use, based on individual-level (Level-1) variables and school-level (Level-2) variables that convey information typically used to characterize school environments1,11,14-16,35,40-42.
Individual-level variables
Individual-level variables included basic demographic information (e.g. age, gender, race/ ethnicity), nicotine dependence, cessation self-efficacy, stages of change, and type of treatment program10,37,38,41-50. Nicotine dependence was constructed using a composite of smoking involvement and nicotine addiction by combining two variables that showed high collinearity: 1) Cigarettes per day (CPD), and 2) Time to first cigarette (TTFC). These two items accounted for the majority of variance in the Fagerström Test for Nicotine Dependence (FTND)51. CPD has traditionally been used as an indicator of smoking involvement and exposure (e.g. pack-years). TTFC has been shown to be highly related to: nicotine dependence, exposure to nicotine and carcinogens in both adolescent daily and non-daily smokers, and cessation outcomes among adolescents36,52-54 (Table 1).
School-level variables
Items selected for the school domain related to school location, school size, school-district size and demographics, and school economic status as derived from the NCES database55-58 (Table 1). Specifically, school demographics included locale, through school name and ZIP code, and was broadly classified as: a) city, b) rural, c) suburban, or d) town; while school size included: a) number of full-time teachers, b) student-teacher ratio, and c) total number of students. School district demographics included: a) percentage of school district population with no high-school diploma, b) percentage of school district population unemployed, and c) percentage of school district population at or below the poverty level. Finally, school economic status included: a) percentage of school eligible for free lunch, and b) percentage of school eligible for reduced lunch.
Analysis
Data within the newly formed socio-spatial database were linked for analyses using the HLM7 software, matching individual- and school-level data on the school identifying codes (i.e. NCES-ID and FIPS)59. Hierarchical Linear Modeling (HLM) analyses were conducted to determine the effect of school-level factors on individual-level cessation treatment outcomes (i.e. failed treatment vs treatment success). Because the outcome variable was dichotomous, Bernoulli models for bivariate outcomes were used. The purpose of these analyses was two-fold: 1) to examine the relationship between an adolescent’s individual risks and cessation treatment failure, while controlling for other variables associated with cessation outcomes (e.g. age, race, gender, treatment group [intensive versus brief]), and 2) to determine if the Level-1 relationships were affected by school-level variables, as shown in Figure 1.
The initial step tested an unconstrained (i.e. null) model to confirm that the variability in the outcome of cessation failure was significantly different from zero. Next, a random intercepts model examined the relationships between the Level-1 predictor/control variables and the outcome. Based on the results of the random intercept model, the model removed any Level-1 predictor/control variables that were not significantly related to the outcome from subsequent analyses. Next, a means-as-outcomes model examined how Level-2 variables predicted the Level-1 outcome (with no Level-1 predictor/Table 2. Participant sample characteristics control variables in the models). Finally, a random intercepts and slopes model explored interactions between the Level-1 and Level-2 variables. All analyses were conducted using HLM7 statistical software59.
Table 2
Participant sample characteristics
| Treatment Success 21.3% (n=1884) | Treatment Failure 78.7% (n=6971) | |||
|---|---|---|---|---|
| LEVEL 1 VARIABLES | % | n | % | n |
| DEMOGRAPHICS | ||||
| Age* | ||||
| 11 | 0.2 | 3 | 0 | 0 |
| 12 | 0.6 | 511 | 0.4 | 27 |
| 13 | 2.5 | 43 | 1.7 | 107 |
| 14 | 11.1 | 193 | 8.6 | 550 |
| 15 | 25.2 | 437 | 23.0 | 1474 |
| 16 | 29.7 | 515 | 29.1 | 1859 |
| 17 | 21.2 | 368 | 25.8 | 1652 |
| 18 | 8.1 | 141 | 10.4 | 665 |
| 19 | 1.2 | 21 | 1.0 | 62 |
| Gender | ||||
| Female | 56.1 | 1054 | 56.3 | 3916 |
| Male | 43.9 | 826 | 43.7 | 3038 |
| Grade* | ||||
| 6 | 0.4 | 7 | 0.2 | 11 |
| 7 | 1.5 | 24 | 0.9 | 49 |
| 8 | 3.7 | 59 | 2.1 | 120 |
| 9 | 26.4 | 418 | 22.9 | 1320 |
| 10 | 29.0 | 460 | 27.2 | 1566 |
| 11 | 24.4 | 387 | 27.4 | 1577 |
| 12 | 14.6 | 231 | 19.4 | 1120 |
| Race* | ||||
| White | 72.3 | 1216 | 79.5 | 4946 |
| African American | 5.7 | 96 | 2.9 | 178 |
| American Indian | 1.7 | 28 | 1.4 | 88 |
| Asian American | 1.2 | 20 | 1.5 | 95 |
| Hispanic | 13.7 | 230 | 9.3 | 576 |
| Native Hawaiian | 0.1 | 1 | 0.4 | 26 |
| Other | 5.3 | 90 | 4.9 | 306 |
| Bi-racial | 0.1 | 2 | 0.1 | 7 |
| CESSATION SELF-EFFICACY | ||||
| Motivation to quit * | ||||
| None | 3.5 | 21 | 6.5 | 181 |
| Low | 13.3 | 79 | 20.2 | 565 |
| Medium | 39.6 | 235 | 45.3 | 1264 |
| High | 29.6 | 176 | 21.4 | 598 |
| Very high | 14.0 | 83 | 6.5 | 182 |
| Confidence to quit* | ||||
| None | 4.2 | 24 | 6.7 | 177 |
| Low | 19.6 | 111 | 26.6 | 702 |
| Medium | 40.5 | 229 | 43.5 | 1146 |
| High | 21.2 | 120 | 16.8 | 443 |
| Very high | 14.5 | 82 | 6.4 | 168 |
| Stages of change* | ||||
| Do not plan to quit smoking in next 6 months | 7.9 | 50 | 17.3 | 555 |
| Plan to quit smoking in the next 6 months | 40.9 | 259 | 45.1 | 1447 |
| Plan to quit in the next 30 days | 30.0 | 190 | 20.1 | 643 |
| Made a serious attempt in past 6 months | 14.7 | 93 | 13.5 | 432 |
| Quit less than 6 months ago | 6.5 | 41 | 4.0 | 128 |
| SMOKING BEHAVIOR | ||||
| Mean | SD | Mean | SD | |
| Nicotine Dependence Composite | ||||
| (TTFC + CPD) Baseline | 24.44 | 19 | 29.97 | 17 |
RESULTS
Adolescent smokers seeking school-based cessation treatment provided the Level-1 data. Participants were moderately addicted daily smokers (M=12.1 CPD for weekdays, SD=11.1; M=18.2 CPD for weekends, SD=13.7). Refer to Table 2 for detailed characteristics among adolescents who experienced successful (21.3%) versus failed treatment (78.7%). Cessation intervention was offered in 807 schools from 5 States over 12 years (1997-2009), serving as the source of the Level-2 data. A total of 346 schools were located in Florida, 11 in North Carolina, 105 in New Jersey, 194 in Wisconsin and 151 in West Virginia. The schools were identified as being located in a city (n=144), rural area (n=187), suburban area (n=268) or a town (n=108). Refer to Table 3 for additional school characteristics.
Table 3
School characteristics
| LEVEL 2 VARIABLES | City N=144 | Rural N=187 | Suburb N=268 | Town N=108 |
|---|---|---|---|---|
| School demographics/economics | ||||
| Full time teachers+ | 77 (37) | 59 (36) | 90 (36) | 52 (22) |
| Student-teacher ratio+ | 17 (3.27) | 15 (3.23) | 17 (7.2) | 16 (2.4) |
| Total student enrolled+ | 1339 (716) | 962 (715) | 1593 (780) | 848 (394) |
| Free lunch eligible | 40% | 34% | 35% | 34% |
| Reduced lunch eligible | 7% | 7% | 7% | 7% |
| School district demographics | ||||
| Per cent of population without high-school diploma | 11.51% | 15.57% | 12.44% | 16% |
| Per cent of population unemployed | 5.8% | 5% | 6.4% | 5% |
| Per cent of population living below poverty level | 20% | 22% | 18% | 24% |
Results showed significant variance in the cessation treatment failure variable by Level-2 group [χ2 (259)=430.0, p<0.001] (Table 4). The interclass correlation (ICC) determined what part of the variance in cessation outcome was attributable to the individual-level (Level-1) and which part was attributable to the group-level (Level-2). The ICC was 0.102, suggesting that 10% of the variation in cessation treatment failure occurred at the school-level and 90% of the variation occurred at the individual-level or elsewhere. Subsequent models were conducted to examine which variables contributed to the explained variance at each level. Given variance at both the individual- and school-levels, the random intercepts model then entered several Level-1 predictor/control variables into the Level-1 model predicting treatment failure. The initial model included the following: 1) age, 2) gender, 3) nicotine dependence (CPD+TTFC), 4) treatment type assignment, and 5) cessation self-efficacy. Based on the initial model run, age and gender were removed as they were non-significant predictors of the outcome. The final random intercepts model suggested that treatment type (β=-0.41, SE=0.10, p<0.001), nicotine dependence (β=0.02, SE=0.01, p=0.01) and cessation self-efficacy (β=-0.4, SE=0.10, p<0.001) all predicted cessation failure. Specifically, as demonstrated previously60,61, intensive treatment (i.e. N-O-T) and greater cessation self-efficacy predicted a higher likelihood of treatment success, while nicotine dependence predicted a greater likelihood of treatment failure.
Table 4
Predictors of cessation self-efficacy and treatment failure by level
Next, the impact of several Level-2 predictors on cessation failure was examined. These models did not include the Level-1 predictors of outcomes (treatment group, nicotine dependence, or cessation self-efficacy). Level-2 model variables included: 1) percentage of school district population with no high-school diploma, 2) percentage of school district population unemployed, 3) percentage of school district population at or below the poverty level, 4) number of full-time teachers, 5) student-teacher ratio, 6) total number of students, 7) percentage of school eligible for free lunch, 8) percentage of school eligible for reduced lunch, and 9) school locale. Results demonstrate that the percentage of school-district population with less than a high-school diploma (β=0.01, SE=0.003, p=0.02) and the student-teacher ratio (β=0.003, SE=0.001, p=0.008) predict cessation failure. Participants in schools in districts with lower rates of residents receiving high-school diplomas and in schools with a high ratio of students to teachers were more likely to experience higher cessation failure rates.
Finally, a random slopes and intercepts model was conducted to examine how Level-2 variables interact with the Level-1 relationship between predictor/controls and cessation treatment failure. Both free lunch eligible (β=0.01, SE=0.001, p=0.001) and reduced lunch eligible (β=0.01, SE=0.0001, p=0.008) interacted with the relationship between cessation self-efficacy and treatment failure (Table 4). Specifically, individuals from schools with higher percentages of free and reduced lunch eligible students were more likely to experience failed treatment regardless of their level of cessation self-efficacy. There were no other significant interactions between Level-2 and Level-1 variables.
DISCUSSION
While findings showed a higher than average percent of adolescents quit (21.3%), most did not report success. The present study found a significant (10%) proportion of the variance in cessation outcomes was attributable to the specific conditions of the school environment, regardless of an individual adolescent’s cessation self-efficacy. Treatment-seeking adolescent smokers in school districts with a large percentage of the population having less than a high-school education were more likely to experience failed treatment. The same was true for adolescents from schools with a higher ratio of students to teachers. Finally, the strength of the relationship between adolescent smokers’ propensity to quit and treatment success was weakened among individuals attending schools with higher percentages of students eligible for free or reduced lunch programs. Free or reduced price lunch eligibility corresponds to US Federal poverty levels, and as such is highly associated with disadvantage.
Taken together, these findings reflect conditions that are well-established indicators of schools that are underfunded and affected by socio-economic disadvantage62. Results are especially meaningful in light of the fact that adolescent smoking is more prevalent in areas of low socio-economic status63,64. Greater treatment failure in individuals that have high needs for tobacco cessation underscores the importance of policy and programmatic scrutiny. The novel finding is not that adolescents in resource-limited school districts are at increased risk of failure but that the likelihood is high despite their individual motivations to quit. This is supported by other research showing that lower SES leads to the development of lower self-efficacy and a lower propensity to quit smoking65. Similarly, measures of disadvantage account for nearly one-third of the class differential in smoking66. The findings suggest that adolescent-focused smoking cessation policies should consider the importance of social and economic context in quitting smoking. Past research would predict that given two adolescents with an identical motivation to quit smoking in a cessation program, the adolescent with the greater belief in his or her ability to quit smoking (i.e. higher cessation self-efficacy) would be more likely to succeed with quitting smoking67. Our findings suggest that it is not that simple and that even with high motivation there is a heightened need for cessation programs to shield individual self-efficacy by buffering adolescents from the proximal effects of school- or area-level socio-economic disadvantage.
Some of the study’s identified school-related factors and conditions are more malleable than others, with implications for policy makers, principals, teachers or other practitioners who implement school-based tobacco cessation programming. A high student-teacher ratio, as was found in the present study, is often an indicator of proportionately underfunded schools or school districts58,68. Demonstrating the impact of school-level socio-economic disadvantage on tobacco cessation programming provides evidence for policy makers to advocate for increased funding in affected school districts, particularly those experiencing a disproportionate burden of tobacco-related health disparities. High teacher workloads may also suggest the need to establish programs to enhance student-teacher relationships as a means to improve student health. Studies show that low-income students who have strong teacher-student relationships have higher academic achievement69,70. Similarly, cessation programming in underfunded schools may need to supplement programs with tailored or ‘wrap-around’ services such as special advisors, adult or peer mentors, or other assigned resources to foster positive relationships among adolescents who enroll in cessation programs. These types of relationships could also have bearing on self-efficacy of disadvantaged students.
Adolescents who attend schools within socio-economically disadvantaged districts are likely to be among adults with less than a high-school education. Evidence suggests that these adolescents in turn may have high exposure to peer and family smoking, and may see tobacco modeled as a means for coping with economic or financial stress71. Therefore, cessation programming may be supplemented with life skills content and coping techniques to buffer the influence of life stressors on adolescent substance abuse72.
A few limitations should be considered when interpreting the findings. Important individual risk factors for continued tobacco use, such as stress and depression, were not measured in this study. Other potentially important individual- and school-level factors, such as student achievement and school activities, also were not captured. Peer level influence was not included due to a lack of data. It is also noteworthy that the menu of tobacco products available today, including electronic cigarettes, were not available or widely used in the US during the course of the original studies. These and other possible risk factors and confounding variables not measured or accounted for in this study warrant caution when generalizing the findings across US adolescents. Further study with the inclusion of additional factors not measured in this study may lead to more or less variance in cessation outcomes explained by the school environment or higher State-level influences. The 10% variance found in the present study is conservative.
Analyses assumed that adolescents who did not attend the 3-month follow-up continued to smoke. The study did not acknowledge reduction as a positive outcome. While we assert the importance of cigarette reduction as an outcome in real-world implementation, this study was explicitly interested in pinpointing reasons for cessation treatment failure. Moreover, because reasons for participant attrition at follow-up (i.e. missing data) were unknown, the analyses applied the most conservative ITT approach by assuming continued smoking. This approach was also consistent with the study goal to explore failed cessation.
A final caution is the periodic collection of census data at 5-year intervals. This approach dictated that the study use census data closest in time to the years in which the trials were conducted. This may seem like an inexact estimation, but the pooled 5-year sample size provides the most reliable estimate for small populations/geographic areas, such as school districts and ZIP codes73. Moreover, despite having data over an extended period of time for temporal estimation, the design remains cross-sectional, and thereby findings shouldn’t be used to draw causal conclusions.
CONCLUSIONS
Other studies9,11,14,74 have investigated the role of the school environment on individual adolescent smoking prevalence but have not pinpointed the predictive contribution of school-district economic disadvantage on an individual’s ability to quit smoking. The current study suggests that specific place-based factors, such as school-level socio-economic disadvantage, may reduce the benefits of tobacco cessation interventions, despite an adolescent’s high level of self-efficacy to quit. Importantly, this finding may be applicable to other school-based wellness programs (e.g. obesity, substance abuse, physical inactivity). To that end, adolescent smoking cessation programming, particularly when school-based, may: a) consider how to buffer the school-level factors that place adolescents at higher risk of failed cessation treatment, and b) be required in greater concentration in locations of socio-economic disadvantage.
Data should not be interpreted to mean that students in poor school districts are doomed to cessation failure. Rather, it draws attention to opportunities to minimize these proximal effects on individual cessation outcomes through tailoring of cessation programs to be cognizant and responsive to these factors.
In summary, the study shed light on the impact that a change in one socio-ecological level can have on a level nested within it. A sociospatial model helped to identify not only the various interactions that occurred at the school-level domain but more precisely what specific factors were the greatest contributors. While 10% may seem small, it represents a part of the environmental landscape that may be modified to improve cessation outcomes. Imagine the improvements in cessation treatment programming if research could likewise uncover or explain the specific contributing domains and factors within those domains for the remaining 90%. Such a vision of tobacco control allows for an active and predictive consideration of multi-level contextual influences on tobacco use related to space and place. It is through this type of approach that we may achieve evidence for the most effective mix of policy, program and economic factors that support or impede tobacco control initiatives. Practitioners and policy makers alike may consider this evidence as supporting the need for policy and practice that are conscious of ‘synchronous’ multi-level influences on adolescent smoking cessation treatment outcomes.