INTRODUCTION
Although the marketplace of tobacco products has changed across time, consumption of tobacco continues to be the chief cause of preventable death in the US1,2. Patterns of youth tobacco use have evolved3, but exposure to tobacco continues to put youths at heightened risk for experimentation and continued use4. Despite this fact, the tobacco industry persists in promoting emerging products to encourage youth uptake5. As a result, concurrent use of two or more tobacco products is of growing public health interest. However, few studies have examined youths’ poly tobacco use6,7, especially among vulnerable groups such as Appalachian youths.
Among youths, e-cigarettes have become the most commonly used tobacco product3, with the most popular combination of products being e-cigarettes and cigarettes7. However, some evidence points to heterogeneity in dual and poly tobacco use by sociodemographic characteristics. For example, dual and poly tobacco use is more prevalent among high schoolers (29.9%) than middle schoolers (11.5%)3. Poly tobacco use has been found to be positively associated with being male and non-Hispanic White relative to single-product use6, and dual and poly tobacco use are more prevalent in rural areas than urban areas in the US8. Additionally, poly tobacco use, relative to single-product use, is associated with greater risk for nicotine dependence and other deleterious health outcomes9,10, warranting investigation of these use patterns among at-risk youth.
Appalachian youths are susceptible to tobacco consumption for several reasons. Factors contributing to Appalachian youth tobacco exposure and use include cultural values that often accept and perpetuate tobacco use and area histories of raising and working with tobacco crops11. Furthermore, the Appalachian region ranks higher in tobacco use and poverty than the national average12,13. With high tobacco use in the region, Appalachian youth often have family members, teachers, and other trusted adults and role models who use tobacco14. In addition, tobacco companies have long targeted rural areas with product marketing and advertising15. Further, rural youth are less often exposed to anti-tobacco campaigns than youth in urban areas15. Sustained tobacco product advertising, community acceptance of tobacco use, and youth exposure to tobacco products and use, combined with less awareness of anti-tobacco messaging, contribute to youth tobacco use rates in the region, which exceed the national average11. Thus, given these contributing factors and overall use rates, Appalachian youths may be vulnerable to dual and poly tobacco use. This study examines prevalence and sociodemographic correlates of single, dual, and poly tobacco use in a sample of Appalachian youths. We aim to determine, specifically, dual and poly use patterns among sociodemographic groups.
METHODS
Study design
We analyzed data from the Youth Appalachian Tobacco Study (YATS) (n=1116). This cross-sectional study was approved by the (University of Louisville) Institutional Review Board and conducted between 2014 and 2016 to examine tobacco use patterns, sources of tobacco exposure, and perceptions and attitudes surrounding tobacco products among Appalachian youth. Middle and high school students in three Appalachian states, Kentucky, North Carolina, and New York, were invited to participate. Tobacco use rates guided the selection of the three states. Youth tobacco use was high in Kentucky, moderate in North Carolina, and low in New York (17.9%, 15.0%, and 10.6%, respectively)16. Students in schools in three Kentucky counties, three North Carolina counties, and two New York counties participated.
Parents or guardians received a letter prior to data collection and could decline their child’s participation; students were given assent forms on the day of data collection in their school and could decline participation. Questionnaires were completed during regular school hours in approximately 40 minutes. YATS is described in more detail elsewhere17.
Measures
Sociodemographic characteristics
We used the following sociodemographic characteristics: gender (male vs female), race/ethnicity, age, school type (middle vs high), state (New York vs Kentucky vs North Carolina), smartphone use (<20 vs ≥20 hours/week), and number of household tobacco users (zero vs ≥1). Race/ethnicity included the following categories: African American, Hispanic, White, Asian, and Other. This variable was dichotomized into White/Caucasian and non-White/non-Caucasian. The number of household tobacco users measure excluded the participant.
Tobacco use
Tobacco products examined were cigarettes, e-cigarettes, and smokeless tobacco. We defined current use as past-month use for each product. We created a pattern of tobacco use variable (i.e. never, former, single, dual, poly) based on exclusive use of each of the included products (single), any combination of two products (dual), and use of all three products (poly). Never users were participants who had never used tobacco. Former users were youth who indicated past, but not current, use of one or more of the included products.
Statistical analysis
We computed prevalence estimates for patterns of tobacco use overall and by sociodemographic characteristics. Using analysis of variance and χ2 tests, we examined characteristics across tobacco use categories. We estimated adjusted odds ratios and 95% confidence intervals for associations between sociodemographic characteristics and patterns of tobacco use (reference: never use) using multivariable multinomial logistic regression. School type was included in the model in place of age to avoid multicollinearity. We analyzed data using SAS 9.4 (Cary, NC).
RESULTS
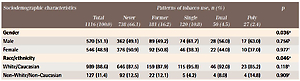
Table 1 displays participant sociodemographic characteristics stratified by tobacco use. The gender distribution was nearly even (51.1% male, 48.9% female). The sample was predominantly White/Caucasian (88.6%). The mean age was 13.7 years (SD=1.9) with a median of 14 years (range: 11–19). The majority of respondents were from North Carolina (46.4%), followed by Kentucky (34.1%) and then New York (19.5%). About one-third (32.8%) used smartphones for ≥20 hours/week, and slightly more than half (57.3%) had households with tobacco users. Nearly a tenth of the sample were single users (10.8%), 4.5% were dual users, and 2.4% were poly users. The most popular dual use groups were cigarettes and smokeless tobacco (2.1%) and cigarettes and e-cigarettes (1.9%) (Supplementary file, Table S1).
Table 1
Participant sociodemographic characteristics by patterns of tobacco use, The Youth Appalachian Tobacco Study (N=1116)
| Sociodemographic characteristics | Total 1116 (100.0) | Never 738 (66.1) | Patterns of tobacco use, n (%) | Poly 27 (2.4) | p | ||
|---|---|---|---|---|---|---|---|
| Former 181 (16.2) | Single 120 (10.8) | Dual 50 (4.5) | |||||
| Gender | 0.036a | ||||||
| Male | 570 (51.1) | 362 (49.1) | 89 (49.2) | 74 (61.7) | 28 (56.0) | 17 (63.0) | 0.756b |
| Female | 546 (48.9) | 376 (50.9) | 92 (50.8) | 46 (38.3) | 22 (44.0) | 10 (37.0) | 0.977c |
| Race/ethnicity | 0.046a | ||||||
| White/Caucasian | 989 (88.6) | 646 (87.5) | 159 (87.9) | 115 (95.8) | 46 (92.0) | 23 (85.2) | 0.118b |
| Non-White/Non-Caucasian | 127 (11.4) | 92 (12.5) | 22 (12.1) | 5 (4.2) | 4 (8.0) | 4 (14.8) | 0.909c |
| Age (years) | <0.001a | ||||||
| Mean ± SD | 13.7 ± 1.9 | 13.3 ± 1.7 | 14.4 ± 1.9 | 14.7 ± 1.9 | 15.1 ± 1.8 | 14.3 ± 1.9 | 0.248b |
| Median (min–max) | 14 (11–19) | 13 (11–19) | 14 (11–19) | 15 (11–19) | 15 (12–18) | 14 (11–18) | <0.001c |
| School type | <0.001a | ||||||
| Middle school | 679 (60.8) | 508 (68.8) | 86 (47.5) | 55 (45.8) | 17 (34.0) | 13 (48.2) | 0.311b |
| High school | 437 (39.2) | 230 (31.2) | 95 (52.5) | 65 (54.2) | 33 (66.0) | 14 (51.8) | <0.001c |
| State | <0.001a | ||||||
| New York | 218 (19.5) | 208 (28.2) | 72 (39.8) | 61 (50.9) | 27 (54.0) | 12 (44.4) | 0.831b |
| Kentucky | 380 (34.1) | 367 (49.7) | 78 (43.1) | 43 (35.8) | 19 (38.0) | 11 (40.7) | 0.009c |
| North Carolina | 518 (46.4) | 163 (22.1) | 31 (17.1) | 16 (13.3) | 4 (8.0) | 4 (14.8) | |
| Smartphone use (hours/week) | <0.001a | ||||||
| <20 | 750 (67.2) | 520 (70.5) | 119 (65.8) | 72 (60.0) | 27 (54.0) | 12 (44.4) | 0.314b |
| ≥20 | 366 (32.8) | 218 (29.5) | 62 (34.2) | 48 (40.0) | 23 (46.0) | 15 (55.6) | 0.217c |
| Household tobacco usersd | <0.001a | ||||||
| Zero | 477 (42.7) | 364 (49.3) | 65 (35.9) | 32 (26.7) | 9 (18.0) | 7 (25.9) | 0.477b |
| ≥1 | 639 (57.3) | 374 (50.7) | 116 (64.1) | 88 (73.3) | 41 (82.0) | 20 (74.1) | 0.001c |
a Chi-squared/Fisher's exact test (categorical) or ANOVA (continuous) p-value comparing never users, single users, dual users, and poly users.
b Chi-squared/Fisher's exact test (categorical) or ANOVA (continuous) p-value comparing single users, dual users, and poly users.
Frequencies of dual and poly use were higher in males, Whites/Caucasians, older participants, and participants living with tobacco users (Table 1). However, compared to dual use, prevalence of poly use was higher in youth who used smartphones ≥20 hours/week and lower in New York residents. Further, the distribution of poly use was nearly even by school type (48.2% middle school). Distributions among never users and any current users varied by all included sociodemographic groups (p<0.05 for all). Conversely, single, dual, and poly use groups did not differ by covariates when examined without never users. Variation between never and former users occurred by factors such as state and number of household tobacco users (p<0.05 for each).
Table 2 shows associations between sociodemographic characteristics and patterns of tobacco use (reference: never use). Associations were found in all characteristics except race/ethnicity for single use. Specifically, females (vs males) had fewer odds of single use (OR=0.59; 95% CI: 0.39–0.89). Dual use was more strongly
Table 2
Multivariable multinomial logistic regression models of associations between participant sociodemographic characteristics and patterns of tobacco use (N=1116)
| Sociodemographic characteristics | Patterns of tobacco usera | |||||||
|---|---|---|---|---|---|---|---|---|
| Former | Single | Dual | Poly | |||||
| AORb | 95% CI | AORb | 95% CI | AORb | 95% CI | AORb | 95% CI | |
| Gender | ||||||||
| Male | Ref. | Ref. | Ref. | Ref. | ||||
| Female | 1.07 | (0.76–1.51) | 0.59 | (0.39–0.89) | 0.76 | (0.41–1.41) | 0.49 | (0.22–1.13) |
| Race/ethnicity | ||||||||
| White/Caucasian | Ref. | Ref. | Ref. | Ref. | ||||
| Non-White/Non-Caucasian | 1.33 | (0.79–2.26) | 0.44 | (0.17–1.14) | 0.99 | (0.33–2.98) | 1.53 | (0.49–4.81) |
| School type | ||||||||
| Middle school | Ref. | Ref. | Ref. | Ref. | ||||
| High school | 2.68 | (1.90–3.78) | 2.68 | (1.77–4.05) | 4.69 | (2.50–8.81) | 2.25 | (1.02–4.98) |
| State | ||||||||
| New York | Ref. | Ref. | Ref. | Ref. | ||||
| Kentucky | 1.95 | (1.19–3.18) | 2.86 | (1.55–5.27) | 5.15 | (1.72–15.44) | 2.19 | (0.67–7.14) |
| North Carolina | 1.13 | (0.71–1.80) | 1.28 | (0.69–2.38) | 2.18 | (0.72–6.64) | 1.22 | (0.37–3.97) |
| Smartphone use (hours/week) | ||||||||
| <20 | Ref. | Ref. | Ref. | Ref. | ||||
| ≥20 | 1.07 | (0.74–1.54) | 1.58 | (1.03–2.43) | 1.75 | (0.94–3.26) | 3.02 | (1.34–6.80) |
| Household tobacco usersc | ||||||||
| Zero | Ref. | Ref. | Ref. | Ref. | ||||
| ≥1 | 1.67 | (1.18–2.37) | 2.31 | (1.48–3.61) | 3.86 | (1.82–8.21) | 2.68 | (1.09–6.57) |
associated with school type, state, and household tobacco users than was former, single, or poly use. For example, youth living in households with at least one tobacco user (vs no tobacco users) had greater odds of former, single, dual, and poly use, and the strength of association was greater for dual use (OR=3.86; 95% CI: 1.82–8.21). Further, Kentucky residents (vs New York) had greater odds of former, single, and dual use, but not poly use. Youths who used smartphones ≥20 hours/week (vs <20 hours/week) had greater odds of single and poly use, but not former or dual use.
DISCUSSION
Our study characterizes patterns of tobacco use in a sample of Appalachian youths. Consistent with prior research, dual and poly use were more prevalent among males, Whites/Caucasians, and older participants3,6,7. We found that dual and poly use differed by state and smartphone use. Specifically, state was associated with former, single, and dual use, and smartphone use was associated with single and poly use. When found to be significantly associated with a sociodemographic factor, dual use had a stronger association than any other use category.
Moreover, living with one or more tobacco user(s) is associated with youth using any tobacco, including use of multiple tobacco products. Previous work with Appalachian youth found significant associations between residing in a household with one or more tobacco users and intention to try a tobacco product18. Other research has documented positive associations between living with a tobacco user and youth use of tobacco products19-22. For example, two recent studies with Appalachian middle school students found, for those who lived in a tobacco-use household, nearly threefold increased odds for dual use23 and an increased likelihood of trying alternative tobacco products (e.g. e-cigarettes, cigarillos)24. Tobacco use by a household member is believed to convey acceptability of product use25, and, especially in Appalachia where overall use rates are high, further normalizes tobacco’s acceptability for youth.
Patterns of youth tobacco use may evolve in conjunction with shifts in the tobacco industry. These changes may lead to increases in dual and poly use with unknown health consequences. For example, e-cigarette use has been found to be associated with subsequent cigarette use in youth4. Youth e-cigarette and cigarette dual users are at higher risk for nicotine dependence9, including higher likelihood of becoming established users as they transition into adulthood26. A recent study in Tennessee, located in the Central Appalachian region, found that more than half of high school students who used e-cigarettes also used at least one other tobacco product27. Another inquiry with Tennessee Appalachian middle school students reported increases over time in dual use23. Taken together, these studies point to increasing public health concerns surrounding Appalachian youth dual and poly tobacco use.
Sociodemographic differences in dual and poly use may drive tobacco-related health disparities. Future research should seek to deepen understanding of sociodemographic factors associated with these tobacco use patterns, especially given possible increases in dual and poly use in vulnerable populations, such as Appalachian youth. For example, although we found that dual use, when significantly related to sociodemographic characteristics, had a stronger association than other tobacco use categories, additional work is needed with larger samples to more fully explicate such relationships and to examine them across time. Further work characterizing use patterns will inform tobacco interventions aimed at preventing and reducing youth tobacco consumption, and such work is especially important with vulnerable populations of youths who are more often targeted by tobacco marketing and more likely to use tobacco products.
Limitations
As with all investigations, our study has limitations. First, participants were assessed on use of cigarettes, e-cigarettes, and smokeless tobacco. However, cigars and hookah are also popular among youths3, and these products are commonly used in certain sociodemographic groups (e.g. African American youth, males). Second, due to the sample size, we could not stratify by specific combinations of use (e.g. cigarette + e-cigarette, smokeless + e-cigarette) and the precision of some estimates was hindered. Future research examining use combinations and incorporating additional products that may be popular with youths would be useful in further investigating these associations. Despite these limitations, our study is among the first to characterize patterns of dual and poly use in Appalachian youth.
CONCLUSIONS
Patterns of tobacco use vary by key sociodemographic characteristics. Specifically, dual and poly use were more prevalent among males, Whites/Caucasians, older participants, and youth living with tobacco users. High schoolers and participants living with one or more tobacco user(s) had greater odds of any tobacco use, including the use of multiple products. Our findings serve as the building blocks for future research that examines sociodemographic disparities in, and downstream health consequences of, dual and poly use among Appalachian youth. As health professionals design prevention messaging, recognizing and addressing concurrent tobacco use is vital.