INTRODUCTION
Smoking, a modifiable factor, is the leading cause of several preventable chronic diseases (such as cancer, cardiovascular diseases, and respiratory diseases), disability, and death. It is responsible for massive direct and indirect costs, including healthcare costs1,2. Smoking is common among vulnerable and socioeconomically disadvantaged groups and is a significant contributor of health inequalities across populations3-5. The prevalence of smoking, including the severity of smoking (i.e. the average number of cigarettes smoked per day), is higher among people with mental disorders than those without mental disorders6,7. This leads to disproportionately higher rates of preventable chronic diseases and deaths in people with mental disorders8. Therefore, although the causal direction between mental disorders and smoking is unclear or complex, people with mental disorders are recognized as an important population group for smoking cessation interventions.
Although most smokers want to quit smoking, many continue smoking as they report that smoking provides them with mental health benefits9,10 . This issue is even more relevant among people with mental disorders as they experience additional barriers to quit smoking11-14. Evidence shows that smoking cessation can be achieved among people with mental illness using the same intervention (behavioral support and pharmacotherapy) that works for the general population15,16. Studies have reported that smoking cessation is associated with mental health benefits, that is, reduction in symptoms of mental illness such as depression, anxiety, stress, and improvement in quality of life17. Despite this evidence, the proportion of people with smoking cessation (thus the decline in smoking) is lower among those with mental illness than the general population6,7,18.
The lower rate of smoking cessation among people with mental disorders may be related to their experience of nicotine withdrawal symptoms during the cessation process, fear that cessation could lead to withdrawal symptoms that they may face, and the perceived benefits of smoking on mental health11-14. Furthermore, they may misinterpret the immediate loss of nicotine withdrawal symptoms after smoking as mental health benefits, and do not act to curb or quit smoking. However, taking actions to quit smoking may also depend on their socioeconomic characteristics, vulnerabilities, and preferences to cessation options19,20. Therefore, smoking cessation interventions adapted to the needs of an individual with mental disorders might have the greatest impact on reducing the number of smokers and addressing the smoking disparities. To be able to do so, it is essential to distinguish specific populations with mental disorders that are less successful in quitting smoking. This study compared the characteristics of current smokers and former smokers with mental disorders, using a nationally representative community sample in Canada.
METHODS
Data source
This is a cross-sectional study that used data from the Public Use Microdata File of the Canadian Community Health Survey-Mental Health (CCHS-MH) 2012, accessed through the University of Calgary webpage (https://library.ucalgary.ca/sands). Detail description of the survey, including data collection methodology, questionnaire, and survey response rate, are available on the website of Statistics Canada21. Briefly, the CCHS is a nationally representative cross-sectional survey conducted by Statistics Canada since 2001. The CCHS collects data on general and contentfocused health status, health behaviors, and healthcare use of the Canadian household populations in a representative sample. The CCHS 2012 was a mental health and well-being content-focused survey of the Canadian household population aged ≥15 years living in the ten provinces (n=25100; n is rounded according to the reporting guidelines of Statistics Canada). This survey excluded people who lived in reserves and any other aboriginal settlements, fulltime Canadian armed forces, and people who lived in institutions, altogether accounting for around 3% of the total Canadian population (CCHS 2012). Given that the Public Use Microdata File of the CCHS is deidentified and publicly available, review and approval by our research ethics board, the Conjoint Health Research Ethics Board at the University of Calgary was not required.
Measures
People with the presence of any mental health disorder, including major depressive disorder, bipolar disorder, mood disorder, hypomania, generalized anxiety disorder, and substance-dependence (includes alcohol and drug dependence) in the last 12 months, were identified for this study. In the CCHS 2012, these mental health disorders were measured (or diagnosed) using the World Health Organization Composite International Diagnostic Interview (WHOCIDI) instrument21. Survey respondents’ self-reported smoking status was classified as current smoker, former smoker, and never smoker. Current smoker includes current daily smokers and current occasional smokers. Former smoker includes former daily smokers and former occasional smokers who stopped smoking completely. Other variables of interest were characteristics of people with any mental disorder. These included sociodemographic characteristics (age, sex, marital status, educational attainment, total annual household income, and immigration status), professional consultations/services received, presence of chronic diseases, and physical activity.
Analysis
The analysis was limited to survey respondents with any mental health disorders (n=2700; n is rounded according to the reporting guidelines of Statistics Canada). The proportion and corresponding confidence interval (95% CI) of people with mental disorders who were former smokers (i.e. quit smoking), current smokers, and never smokers, were calculated. Bivariate analysis was done to examine the differences in the distribution of characteristics of people with mental disorders across the groups of former smokers, current smokers, and never smokers. The distribution of characteristics, specifically professional consultations/services received, presence of chronic diseases, and physical activity was not different by smoking status among people with mental disorders. These variables were then excluded in the subsequent analysis.
The sociodemographic characteristics, namely age, sex, marital status, educational attainment, immigration status, and total household income status, were further analyzed. The association between these characteristics and smoking status was examined using unadjusted and adjusted multivariable logistic regression analysis. First, we developed logistic regression models in the whole sample, separately for two different smoking outcomes: one being continuing smoker vs nonsmoker and the other being former smoker vs never smoker. To enable us to make a direct comparison between sociodemographic characteristics of former smokers and current smokers, we then developed logistic regression models in the restricted sample of ever smokers (n=2000; n is rounded according to the reporting guideline of Statistics Canada). Unadjusted models were developed for individual characteristics. Adjusted models were developed, including all these characteristics in the same model, where every estimated odds ratio (AOR) with 95% CI was adjusted for every other variable in the model (simultaneous adjustment). In order to compare the findings between those with and without mental disorders, the same models were developed among people without mental disorders as well.
The CCHS survey used stratified, multistage sample selection techniques, which included clustering and unequal selection probabilities. Survey sampling weights and coefficients of variation, provided by Statistics Canada, were used to ensure the representativeness of the target population and to account for the design effects. All estimates were calculated applying weights, and the CIs for proportions were calculated using the coefficient of variation to compute the margin of error. All analyses were performed using STATA/IC version 14.1. An alpha level of 5% and the inclusion of null value within the 95% CIs was used to assess statistical significance.
RESULTS
Table 1 describes the smoking and sociodemographic characteristics of the survey respondents with the presence of any mental disorders. Of the total 2700 respondents, 37.5% (95% CI: 34.0–41.0) were current smokers, 33.6% (95% CI: 29.8–37.4) were former smokers, and 28.8% (95% CI: 25.4–32.2) were never smokers. The majority of respondents were aged ≤45 years, males, single or never married (includes either widowed or divorced or separated or single), postsecondary graduates, had annual household income ≥$60000 (CA$), and were non-immigrants (Table 1).
Table 1
Characteristics of people with any mental disorders, Canada 2012 (N=2700)
Table 2 illustrates the distribution of sociodemographic characteristics of people with any mental disorders across their smoking status. Among current smokers, 31.2% (95% CI: 26.4–36.0) were aged 15–24 years, 45.8% (95% CI: 39.6–52.0) were females, and 66.3% (95% CI: 58.5–74.1) were single or never married. Similarly, 59.6% (95% CI: 52.6–66.6) of smokers had less than post-secondary education, 12.1% (95% CI: 8.3–15.9) had household income ≤$20000, and 12.1% (95% CI: 7.8–16.4) were immigrants. Whereas, among former smokers, 21.1% (95% CI: 16.2–26.0) were aged 15–24 years, 43.2% (95% CI: 37.0–49.4) were females, and 49.3% (95% CI: 42.6–56.0) were single or never married. Similarly, 37.7% (95% CI: 31.2–44.2) of former smokers had less than post-secondary education, 7.2% (95% CI: 4.0–10.4) had household income ≤$20000, and 8.4% (95% CI: 4.9–11.9) were immigrants.
Table 2
Characteristics of people with any mental disorders across smoking status, Canada 2012 (N=2700)
| Characteristics | Current % (95% CI) | Smoking status Former or quitted % (95% CI) | Never % (95% CI) |
|---|---|---|---|
| Age (years) | |||
| 15–24 | 31.2 (26.4–36.0) | 21.1 (16.2–26.0) | 35.9 (30.1–41.7) |
| 25–34 | 23.0 (17.2–28.8) | 19.3 (13.5–25.1) | 18.9 (13.2–24.6) |
| 35–44 | 16.7 (11.7–21.7) | 16.4 (11.4–21.4) | 17.1 (11.5–22.7) |
| 45–54 | 16.1 (11.1–21.1) | 20.1 (14.1–26.1) | 12.4 (7.5–17.3)a |
| 55–64 | 10.5 (6.4–14.6)a | 14.5 (9.5–19.5)a | 9.8 (5.3–14.3)a |
| ≥65 | 2.4 (1.1–3.7)a | 8.4 (5.8–11.0) | 5.8 (3.5–8.1)a |
| Sex | |||
| Male | 54.2 (47.8–60.6) | 56.8 (50.1–63.5) | 43.3 (36.1–50.5) |
| Female | 45.8 (39.6–52.0) | 43.2 (37.0–49.4) | 56.7(49.7–63.7) |
| Marital status | |||
| Married/Common law | 33.7 (27.6–39.8) | 50.7 (44.4–57.0) | 38.6 (32.0–45.2) |
| Widow/divorced/separated or single | |||
| Education status | 66.3 (58.5–74.1) | 49.3(42.6–56.0) | 61.4(53.8–69.0) |
| Less than post-secondary | 59.6 (52.6–66.6) | 37.7 (31.2–44.2) | 42.0 (35.0–49.0) |
| Post-secondary graduated | 40.4 (34.6–46.2) | 62.3 (54.9–69.7) | 57.9 (50.7–65.1) |
| Income status (CA$) | |||
| No or <20000 | 12.1 (8.3–15.9) | 7.2 (4.0–10.4)a | 5.9 (2.7–9.1)a |
| 20000–39999 | 19.3 (13.9–24.7) | 11.8 (7.6–16.0)a | 14.4 (9.3–19.5)a |
| 40000–59999 | 18.9 (13.6–24.2) | 16.6(11.8–21.4) | 18.9 (13.6–24.2) |
| 60000–79999 | 13.8 (9.5–18.1) | 22.2 (17.0–27.4) | 16.1 (11.2–21.0) |
| ≥80000 | 35.9 (30.2–41.6) | 42.1 (35.6–46.6) | 44.7 (37.8–51.6) |
| Immigration | |||
| Yes | 12.1 (7.8–16.4)a | 8.4 (4.9–11.9)a | 23.2 (23.2–29.5) |
| No | 87.9 (81.4–94.4) | 91.6 (87.8–95.4) | 76.9 (70.0–83.8) |
| Moderate/vigorous physical activity | |||
| Yes | 71.2 (64.8–77.6) | 74.3 (67.6–81.0) | 4.6 (67.9–81.3) |
| No | 28.8 (22.9–34.7) | 25.7 (19.8–31.6) | 25.4 (19.6–31.2) |
| Chronic condition | |||
| At least one | 58.5 (51.6–65.4) | 59.3 (52.3–66.3) | 56.9 (49.8–64.0) |
| None | 41.5 (35.5–47.5) | 40.7 (34.4–47.0) | 43.1 (35.9–50.3) |
| Mental health consultation | |||
| Yes | 43.3 (37.1–49.5) | 45.4 (38.9–51.9) | 47.4 (40.1–54.7) |
| No | 56.7 (50.0–63.4) | 54.6 (48.2–61.0) | 52.6 (45.7–59.5) |
Table 3 shows the association between sociodemographic characteristics and smoking status of people with mental disorders. The odds of smoking were significantly higher among those who were aged 25–64 years compared to those aged ≥65 years (AOR=2.6–3.4) and those who had less than post-secondary education compared to those who had post-secondary education (AOR=2.3, 95% CI: 1.6–3.2). Also, the odds of smoking were significantly higher among those with household income ≤$20000 compared to those with ≥$80000 (AOR=2.7, 95% CI: 1.5–2.4). The odds of smoking among females compared to males (AOR=0.6, 95% CI: 0.4–0.8) and among immigrants compared to Canadian born (AOR=0.5, 95% CI: 0.3–0.7) were significantly lower. The odds of quitting smoking among those aged 15–24 years compared to those aged ≥65 years (AOR=0.3, 95% CI: 0.2–0.7) was significantly lower. Similarly, the odds of quitting smoking among females compared to males (AOR=0.5, 95% CI: 0.4–0.7) and among immigrants compared to Canadian born (AOR=0.2, 95% CI: 0.1– 0.4) were significantly lower.
Table 3
Association between characteristics of people with any mental disorders and their smoking status, Canada 2012 (N=2700)
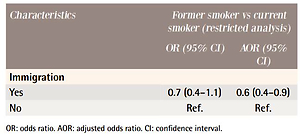
Table 4 illustrates the association between sociodemographic characteristics of people with mental disorders and their smoking status, restricted to ever smokers only. The findings from this restricted sample analysis are similar to the findings in Table 3 that resulted from the full sample analysis, including ever smokers and never smokers. Respondents aged <65 years compared to those who were <65 years were significantly less likely to quit smoking (AOR=0.2–0.3). Similarly, immigrants (AOR=0.6, 95% CI: 0.4–0.9), those with less than post-secondary education (AOR= 0.4, 95% CI: 0.3– 0.6), and those who were single or never married (AOR=0.6, 95% CI: 0.4–0.9) were less likely to quit smoking. Although the estimates of OR failed to reach statistical significance in some of the categories of income (probably lacked power due to small sample size), we can still see a pattern in them that as the income level increases, people are relatively more likely to quit smoking (in comparison to the highest income group). Overall, the patterns of association between sociodemographic characteristics and smoking status (former vs current smoker) among people with mental disorders were similar to those without mental disorders. Notably, those with less than post-secondary education and immigrants were more likely to continue smoking if they had mental disorders (Supplementary file, Table S1).
Table 4
Association between characteristics of people with any mental disorders who were ever smokers and their smoking status, Canada 2012 (N=2000)
DISCUSSION
This cross-sectional study examined the characteristics of current smokers and former smokers with mental disorders, using the nationally representative community-based data in Canada. This study found that a higher proportion of people with mental disorders were current smokers (37.5%) than former smokers (33.6%). Among the people with mental disorders, immigrants (compared to Canadian-born group) and those who were single or never married (compared to married or living with a common-law partner) were less likely to quit smoking by 40%. Similarly, people with less than post-secondary education and those who were young and middleaged adults were less likely to quit smoking than postsecondary graduates and elderly.
Consistent with our study findings, other studies have found a disproportionately higher prevalence of smoking and a lower prevalence of quitting among those who have a mental illness than the general population22-24. In 2019, the prevalence of current smokers was 15% and that of former smokers was 26%, in the general Canadian population22. In our analysis of people with no mental disorders, we found 19.1% were current smokers and 39.3% were former smokers. In the UK, among groups with and without mental illness, the prevalence of current smokers was 34.1% and 22.3%, respectively, and the prevalence of former smokers was 49.4% and 66.2%, respectively25.
Importantly, our study findings provide insight into the socioeconomic characteristics of people with mental disorders who continued or quit smoking. The observed socioeconomic differences in smoking cessation were similar between people with and without mental disorders and are consistent with previous findings on people with mental illness and in the general population6,26,27. The disproportionally high number of smokers in the group with mental disorders, along with the socioeconomic disparities, indicates that existing smoking cessation programs are not sufficiently able to meet the smoking cessation needs of vulnerable populations. People with mental disorders have many of the same barriers for smoking cessation as people with no mental disorders, such as fear of withdrawal, weight gain, and cessation failure11,14. However, evidence also suggests that people with mental disorders face additional challenges11-14.
People with mental disorders are more likely to be severe smokers, have high levels of nicotine exposure and dependence, and experience severe nicotine withdrawal symptoms than people with no mental disorders12,13. Hence, they face more considerable difficulties in quitting smoking. Additionally, people with mental disorders choose to smoke as a self-medication to cope with the effects of mental disorders11, a practice that has been positively reinforced due to the widely held belief that smoking benefits mental health. Health professionals may also hesitate to intervene if they believe that stopping smoking is detrimental to their mental health28. As a result, people with mental disorders are less successful in quitting (or sustained abstinence), and their smoking cessation need remains unmet. However, it is important to realize that although people find smoking (self-medication) helpful in immediately relieving the symptoms of anxiety or depression, it creates the false perception that smoking has psychological benefits; this may be part of the nicotine withdrawal feedback mechanism. It is smoking that causes the psychological disturbances in the first place. Strong evidence suggests that cessation in fact improves mental health17.
The unmet smoking cessation needs of people with mental disorders are even worse in those who are socially deprived, such as people who are less educated, have low incomes, and are immigrants, as they face a less supportive environment that makes their smoking cessation more challenging. The challenges include less access to cessation support (due to, for example, financial constraints, language barriers, less access to resources for cessation, and less knowledge about smoking cessation support measures) and low family or social support3,4,27. Additionally, the high levels of nicotine exposure and dependence, and the severity of mental disorders in this group may make their smoking cessation process less successful29. And, this disappointment could worsen their mental health status30,31. Nonetheless, the occurrence of disparities within the population with the same clinical condition (mental disorders) who are at increased risk for smoking behavior, and the additional disparities among immigrants and less educated people with mental disorders compared to those with no mental disorders, is intolerable.
This study raises important research questions: why people with certain characteristics were (or were not) successful in quitting smoking than others, and why the immigrants and less educated people with mental disorders were particularly less successful in quitting than those without mental disorders. Future studies performing the prospective longitudinal assessment of mental disorders, including the severity, smoking behaviors, cessation attempts, and nicotine withdrawal syndromes among advantaged and disadvantaged people with mental disorders, may provide a clear understanding of the mechanism between mental disorders and cessation. Similarly, in-depth examination of multilevel barriers and enablers for smoking cessation (individual, interpersonal, socioenvironmental, cessation support programs and practices) experienced by those groups may help clarify their vulnerabilities and needs. The findings from these analyses will eventually guide the design and implementation of cessation interventions that meet the cessation needs of vulnerable populations. We were unable to analyze any of these due to data limitations.
Our finding on the characteristics of people with mental problems who are less likely to quit smoking is important for public health workers, including decisionmakers or policymakers. The finding will guide them in allocating resources for research and the design of cessation interventions or the cessation service practices focusing on those people. As the disadvantaged population with mental disorders who smoke represents a subset of smokers, they require specialized cessation support. Populationbased smoking cessation interventions help reduce the smoking prevalence at the population level and improve overall population health32,33. However, not everyone benefits equally from these interventions and instead, sometimes increase the health disparities. Population at-risk cessation intervention approaches target to reduce the smoking exposure for individuals at higher risk, but do not address the disparities between the socially defined groups32,33. This justifies or necessitates the use of a vulnerable population approach for smoking cessation. This approach aims to decrease the smoking-related inequalities by using tailored, personalized smoking cessation strategies that are responsive to their cessation needs, and changing the social conditions that make the vulnerable population at higher risk of continuing smoking33. A significant proportion of people, specifically disadvantaged people, experience mental health concerns in their lifetime and smoking behavior is highly concentrated in this group. The vulnerable population-based cessation intervention approach might be beneficial to diminish the smoking-related disparities, and also to reduce the overall burden of smoking. For example, integrating smoking cessation support into the existing mental health services and tailoring it to the needs of the vulnerable population seem crucial.
Strengths and limitations
This study has several strengths and limitations, which need to be acknowledged to be able to make inferences from the findings. This study analyzed data from the nationally representative community samples, leading to considerable generalizability of the study findings in the Canadian general population. Important to note that 3% of the total Canadian population that represents people living in reserves, full-time members of Canadian forces, residents of remote areas, and residents of health institutions, were not included in this survey. These populations are in fact more vulnerable to mental disorders and social disadvantages. While the inclusion of this population may not change our findings given the small proportion they represent, the findings are not generalizable to this specific population. The survey measured a wide range of mental disorders (major depressive disorder, bipolar, mood disorder, hypomania, generalized anxiety disorder, and substance dependence) using a standardized tool. However, we analyzed the presence of any mental disorders that include these mental disorders; hence, our findings are less specific to a particular mental disorder.
Similarly, as the data on smoking status were based on self-report, smoking status may have been misclassified. The variations in characteristics of people with any mental disorders who smoke and quit are possibly related to the differences in severity of mental disorders. Some of our estimates, mainly, the estimates corresponding to age, income, and immigration, should be interpreted with caution due to the associated high sampling variability attributable to a small sample size.
CONCLUSIONS
This study found that the characteristics of people with mental disorders differ in current smokers and former smokers. Smoking cessation was low in young people, people living without partners or spouses, less educated people, and immigrants, compared to their respective counterparts. The observed socioeconomic disparities in smoking cessation among people with mental disorders may be related to the additional barriers or vulnerabilities experienced by the socioeconomically disadvantaged population. As opposed to the population-based and population atrisk intervention approaches, the targeted smoking cessation approach for the vulnerable population enables the design and implementation of smoking cessation programs targeted to the smoking cessation needs of vulnerable groups, which might be beneficial to reduce the disparities. Future research aiming to improve the understanding of why disadvantaged people with mental disorders choose to continue smoking will be valuable to inform cessation interventions specific to vulnerable populations.