INTRODUCTION
Cigarette smoking and contact with secondhand smoke are the two main preventable risk factors for developing heart and lung diseases, as well as many cancers such as liver and colorectal cancer1,2. Despite the associated risks, 5.5 million Canadians continue to smoke, and it has been estimated that approximately 47000 of these people die annually from smoking-related diseases3. Data collected by Health Canada in 2012 showed that over 18% of all deaths in Canada were attributable to smoking and secondhand smoking4.
Current data have demonstrated that Chinese communities in Canada may smoke at lower rates than the non-immigrant population5-7; however, among current Canadian newcomer smokers, Chinese males smoke more cigarettes per day than any other immigrant group7,8. Despite the lower rates of smoking reported among the Chinese immigrant population, many policy-makers view this issue as problematic and important public health concern, given that Chinese immigrants are the fastest growing immigrant community in Canada, and their pre-immigration smoking behaviors and perceptions may increase the likelihood that they continue their smoking habit in Canada9,10.
Despite showing the willingness to quit smoking among current smokers from the Chinese community7,11,12, most individuals who have made attempts to quit or reduce their smoking behaviors have reported failures in behavior to do so, mainly due to a lack of smoking cessation resources that are competent with their language or cultural norms13,14. To our knowledge, very few resources that provide a linguistically appropriate smoking cessation program for Chinese Mandarin and Cantonese speaking smokers in British Columbia (BC), Canada, including the Greater Vancouver Area (GVA), are currently available. A practical smoking cessation program for ethno-cultural communities should not only be culturally sensitive, but should also provide services in line with their cultural norms, beliefs, and values about smoking and smoking cessation14-19. Numerous studies suggest that such an approach would increase the likelihood of acceptance of the program by the target community and may enhance effectiveness5,16-19.
METHODS
Purpose
The primary purpose of this study was to evaluate the effectiveness of using a culturally and linguistically sensitive smoking cessation educational program towards reducing the smoking behaviors of Chinese-speaking Canadian smokers. We further sought to evaluate whether smokers’ risk perception of smoking was affected by the program, in particular the perceptions of their self-confidence in quitting and the general importance of quitting. A secondary purpose, within the study’s broader aim, was to assess whether supplementing the educational program with culturally and linguistically sensitive one-on-one counseling sessions would differentially affect smoking behaviors and risk perceptions, compared to the educational program alone. Finally, we further decided to include an English-speaking group to our study design, to serve as a comparison group for the Chinese-oriented program.
Study design
A quasi-experimental study design was utilized to best address the purposes of the study. Participants were allowed to select whether they would receive the educational program alone, or whether they received the program with supplemental counseling. Participant data were collected at the beginning and at the end of the 6-month intervention period. These parameters were employed for both the Chinese- and English-speaking groups. Hence, the study employed a mixed-factorial design, in which the initial versus last measurements served as a within-subjects factor and the counselling versus non-counselling groups and Chinese-speaking versus English-speaking groups served as between-subjects factors. Taken together, this approach yielded a 2×2×2 mixed-factorial design.
Sample and sampling procedures
Eligibility criteria for the study were: 1) English-speaking or immigrants of Chinese descent; 2) conversed in either Cantonese, Mandarin, or English; 3) smoked five cigarettes a day or more (self-reported); 4) aged >19 years; 5) willingness to participate in the study for eight months; and 6) interested in smoking cessation. Recruitment methods included community flyers, ads in local Chinese newspapers, outreach to community centers, and recruitment from the Lung Centre at Vancouver General Hospital. The recruitment flyer provided information to potential participants on how to contact the research staff if they were willing to participate in the study and an initial visit date was then arranged.
Overall, 81 individuals expressed their interested to participate in the study, from which 70 (20 females and 50 males) smokers were enrolled and completed the intervention. Eleven participants were excluded due to ineligibility, conflict of time, or distance issues (e.g. lack of transit).
Outcome materials
In the absence of a well-established smoking-related behavioral modification questionnaire in Chinese, risk perceptions measures were drawn from a previously established smoking questionnaire where items had been used successfully with Mandarin and Cantonese smokers in our other studies13,15. Some modifications were applied to include risk perceptions and self-efficacy items, per suggestions we received from a group of 14 healthcare professionals (e.g. primary care physicians, respirologists, and respiratory educators) who reviewed the measurement tool and provided their comments. We sought to measure participants’ perceived risk and benefits of continued smoking, perceived susceptibility to smoking-related diseases, and perceived effectiveness of participation in a culturally relevant smoking cessation program. As part of their evaluation using the questionnaire, participants were also administered a spirometry test of their exhaled carbon monoxide (CO) level (ppm)20.
From the data we collected, four dependent variables were of primary interest for this study, two of which pertained to smoking behaviors and two which pertained to perceptions related to quitting. The smoking behavior variables included exhaled carbon monoxide levels and the number of cigarettes participants’ self-reported smoking per day. The perception variables asked participants to rate on a scale, 1 (lowest) to 10 (highest), their confidence in quitting or cutting down smoking, as well as how important they believed quitting or cutting down to be.
Educational program materials
Take-home educational materials included video clips and written pamphlets in the participants’ preferred language (Mandarin, Cantonese, or English) and were pilot tested with smokers from the target communities for relevance, accuracy, and acceptability. Communication barriers and style, social aspects of smoking, related beliefs, and values corresponding to Mandarin and Cantonese cultural practices were also considered. More details of the educational materials development can be found in a previous publication21. As part of the educational program, participants also completed a triggers and withdrawal symptoms checklist to help monitor their progress throughout the program intervention. Divergent cultural norms and practices between the three target language groups were taken into consideration in the design of the consultations and educational supplements. The study was enriched by inclusion of community engagement, social support, and self-efficacy concepts to facilitate quitting smoking22,23.
Procedures
The study was conducted at the University of British Columbia (UBC) in Vancouver, Canada, between May 2018 and June 2019. Prior to the implementation of the research, a needs assessment study and preliminary research that focused on smoking cessation within ethnic minority communities were conducted between 2012 and 2016, and reports from these studies have been published13,15,16.
Upon their first visits, the aims and processes of the study were explained to the participants, and all participants signed an informed consent form prior to enrollment. After completing a baseline assessment questionnaire, the participants were assigned into a group of their choice: a counseling group or a non-counseling group. Both groups completed the baseline initial assessment (i.e. the questionnaire and spirometry assessment), received take-home educational materials and education on how to use the materials, as well as a triggers and withdrawal symptoms checklist and instructions to complete weekly at home. At the baseline visit, all participants were offered nicotine replacement therapy (NRT) if requested. For both study groups, a final 6-month in-person assessment was conducted at the end of the intervention. In addition, a postintervention follow-up phone assessment was made at 8 months after the participants’ initial visit to assess the participants’ smoking status, possible relapse behaviors, and their self-confidence level towards smoking cessation.
Participants in the non-counseling group received take-home educational materials and received three phone follow-up assessment calls after the baseline assessment at 1-month intervals to monitor their smoking cessation progress. It should be noted that during these follow-up assessment phone calls no counseling services were administered. Telephone calls were approximately 15–30 minutes in length.
The non-counseling group phone calls mainly checked participants’ cravings, symptoms, and quit plan and responded to their smoking cessation-related questions. During each telephone follow-up, a member of the research team administered a checklist of questions regarding cessation progress and perceptions that participants responded to verbally and in their preferred language. A bilingual member of the research team translated participants’ responses on the checklists for Chinese-speaking participants.
The counseling group received four culturally appropriate one-on-one consultations delivered in their preferred language by health professionals from their culture and language group. The consultation sessions were tailored to each participant’s specific needs and smoking habits and a comprehensive ‘Case Profile’ was developed for each participant at the end of the consultation sessions. The in-person consultation sessions for the counseling group addressed the target communities’ values, norms, and beliefs about the benefits of smoking cessation, perceived challenges in planning ‘quit smoking journey’ approaches to control smoking triggers and withdrawal symptoms by modifying routine habits and behaviors, risk perception theories, as well as attempted to improve their self-confidence towards quitting. Each in-person consultation took around 45–60 minutes to complete. Although the aim of the intervention was to be as systematic as possible, we endeavored to allow the counselors and participants to apply some flexibility in timing, discussion topics, and the contents of the consultations. We viewed such flexibility as a potentially important component of our culturally sensitive approach. During the first consultation session, the counselor established a rapport with the participant, reviewed the goals and anticipated outcome of the project, and if needed, modified the consultation procedure based on the participant’s smoking pattern and sociocultural issues. For instance, if a young smoker reported to likely smoke due to social stimulus with friends and colleagues rather than habitual cues, the subsequent consultation sessions were tailored to address the social inducement of their smoking pattern and habits. Likewise, if personal health or the health of family members were major concerns, greater emphasis was given on providing educational and consultation information on these topics during the subsequent consultations.
At the end of the first consultation session, each participant was provided with a checklist to take home and report his or her daily cravings, moods, and withdrawal symptoms. The checklist was then reviewed in the following consultation visit and the counselor provided practical approaches to help minimize the incidents and help the participant to formulate a specific practical quit journey. The subsequent consultation session was scheduled approximately 30 days after the first consultation, and the same pattern was continued until the end of study. During the subsequent consultation sessions, the counselor placed emphasis on motivating the participant to set a ‘quit date’. Part of our culturally sensitive smoking cessation intervention was to involve supportive family members or next-of-kin in the participant’s quit journey.
Data analytic procedures
In congruence with the study’s 2 (condition: counseling vs non-counseling) × 2 (language spoken: Chinese vs English) × 2 (time: initial vs last measurements) mixed-factorial design, a mixed-factorial analysis of variance (ANOVAs) was conducted for each of the four outcome variables. Thus, four ANOVA analyses were conducted. This statistical procedure allowed us to not only assess the effects of each of the independent variables individually, but also allowed us to assess any interactions were present among the factors (e.g. if counseling mattered differential for a particular language group).
Participants were excluded from analyses if they were missing data relevant to the particular analysis. Statistical analyses were conducted using the open-source language R24. Outliers were removed for all analyses, using the ‘outliers’ package in R. To calculate changes in outcomes, we subtracted participants’ initial assessment scores from the last measurements of those variables, where a participant’s last measurement was determined by taking their most recent measurements on either the final assessment or a last previous consultation. Due to smaller number of participants in Mandarin and Cantonese communities (compared to the English mainstream community), as well as the linguistic and cultural dynamics between the two Chinese languages, we combined these languages to make a group to compare the results between English- and Chinese-speaking smokers.
RESULTS
Seventy smokers (30 Chinese, 40 English; 50 males, 20 females) completed the study. To assess the effectiveness of the culturally relevant interventions across language groups over time, 2 (condition: counseling vs non-counseling) × 2 (language spoken: Chinese vs English) × 2 (time: initial measurement vs last measurement) mixed factorial analyses of variance (ANOVAs) were conducted for each of the four outcome measures. Due to smaller number of participants in Mandarin and Cantonese communities (compared to the English mainstream community), as well as the linguistic and cultural dynamics between the two Chinese languages, we combined these languages to make a group to compare the results between English- and Chinese-speaking smokers. Descriptive statistics corresponding to all mixed-factorial ANOVAs are presented in Table 1.
Table 1
Descriptive statistics corresponding to the mixed-factorial analyses of variance, University of British Columbia, Vancouver, BC, Canada, 2018
[i] The ‘Initial’ time of measurement refers to the first measurement collected in the study. The ‘Last’ time of measurement refers to the final measurement collected in the study. The duration between the initial and last measurements may vary among participants due to instances of attrition. For most participants, the last measurement was collected between six and eight months after the initial measurement. Carbon monoxide levels are given in parts per million (ppm). The importance ratings reflect participants ratings of the importance of quitting or reducing their smoking behaviors, on a scale of 1 to 10. The self-confidence ratings reflect participants’ ratings of their self-confidence in quitting or reducing their smoking behaviors, on a scale of 1 to 10.
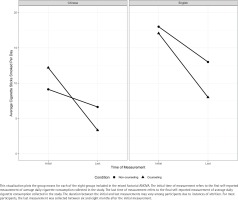
Cigarette consumption
For the number of cigarettes smoked per day outcome variable, no significant interactions were observed. However, significant main effects were observed for both the language [F(1; 86)=12.909, p<0.001, ηp2=0.131] and time [F(1; 86)=11.017, p=0.001, ηp2=0.114] variables (Table 2). These findings suggest that both Chinese- and English-speaking participants significantly decreased their cigarette consumption at nearly equal rates, on average, and that the English-speaking participants, on average, smoked significantly more cigarettes than the Chinese-speaking participants did, across both the initial and final measurement time points (Figure 1). Notably, no significant interactions or main effects related to the study conditions (counseling vs non-counseling) were observed. The mean reduction of cigarettes smoked per day for the English-speaking group was 8.12 cigarettes (SD=6.43), while the mean reduction for Chinese-speaking participants was 7.70 cigarettes (SD=5.70). Taken together, these findings suggest that while general differences in smoking consumption exist between the Chinese- and English-speaking groups, both, on average, significantly reduced the number of cigarettes consumed per day, and that the counseling intervention had no statistically meaningful effect towards that reduction.
Table 2
Significant results from the mixed-factorial analyses of variance, University of British Columbia, Vancouver, BC, Canada, 2018
[i] All findings reflect main effects with the exception of the ‘Counseling X Language’ result, which reflects an interaction effect. ηp2 is the partial eta-squared effect size. Carbon monoxide levels reflect parts per million. The main effects for ‘Language’ reflect the comparisons of the Chinese and English versions of the treatments. The ‘Time’ main effects reflect the comparisons between the initial and l’st measurements for a given dependent variable. The ‘Initial’ time of measurement refers to the first measurement collected in the study. The “Last’ time of measurement refers to the final measurement collected in the study. The duration between the initial and last measurements may vary among participants due to instances of attrition. For most participants, the last measurement was collected between six and eight months after the initial measurement.
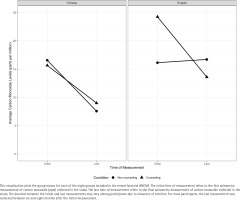
CO levels
Similar to cigarettes smoked per day, no significant interactions were found for the CO outcome variable, although significant main effects were again found for both the language [F(1; 94)=7.963, p=0.006, ηp2=0.078] and time [F(1; 94)=6.999, p=0.01, ηp2=0.069] variables. However, there was not a significant main effect for the counseling variable (Figure 2). Also, similar to cigarettes smoked per day, average levels of CO decreased nearly equally for the English-speaking (mean decrease=7.74 ppm, SD=13.14) and Chinese-speaking (mean decrease=7.32 ppm, SD=6.23) groups (Table 2). As the findings related to cigarettes smoked per day, these findings suggest the program may have contributed to a significant reduction in CO levels, but that this reduction is not affected by supplemental counseling.
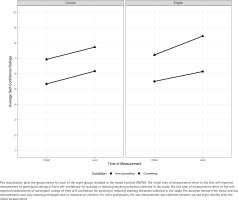
Importance of quitting and self-confidence level
For the self-reported ratings of the importance of quitting and participants’ confidence in quitting, a different pattern of findings was observed. For the importance ratings, a significant interaction was observed between the counseling condition and language variables [F(1; 82)=4.482, p=0.037, ηp2=0.052], with an additional significant main effect observed for the language variable in isolation [F(1; 82)=9.240, p=0.003, ηp2=0.101]. The significance of the interaction appears to be driven by the differential increase in self-rated importance of quitting between the counseling and non-counseling interventions within the Chinese-speaking group (Table 2 and Figure 3). For Chinese-speakers in the non-counseling group, a mean increase of zero was observed (SD=1.58), whereas the Chinese-speakers in the counseling group saw an average increase of 0.73 (SD=1.10). For English-speakers in the noncounseling group, a mean increase of 0.33 (SD=0.82) was observed, whereas the English-speakers in the counseling group only showed a mean increase of 0.25 (SD=0.73) over time. Towards the main effect, the Chinese-speaking group increased their importance ratings (mean increase=0.55, SD=1.23) by nearly twice that of the English-speaking participants (mean increase=0.27, SD=0.74), when the counseling condition variable is not considered (Table 1). These findings suggest that the supplemental counseling led to increases in importance ratings compared to the non-counseling group, but only for the Chinese-speaking participants. English-speakers saw no effect of counseling on importance ratings because in both the counseling and non-counseling groups their ratings were equally high.
Figure 3
Three-way mixed-factorial ANOVA interaction plot exploring participant ratings of the importance of quitting or reducing smoking behaviors
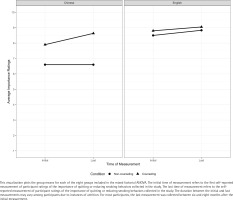
Finally, for the ratings of confidence in smoking cessation, significant main effects were observed for the counseling condition [F(1; 86)=12.336, p<0.001, ηp2=0.125], and time variables [F(1; 86)=4.217, p=0.043, ηp2=0.047]. Towards the main effect of condition, the average increase for the counseling group was 1.04 (SD=2.37), while the non-counseling group increased by an average of 0.73 (SD=2.42). Regarding the time main effect, when the full sample is considered, the average confidence ratings increased by 0.96 (SD=2.36) (Table 2 and Figure 4). These findings suggest that overall, the counseling condition had higher average self-confidence ratings across both time points, yet the supplemental counseling did not differentially affect how much change occurred over time. The language groups did not statistically differ for this variable.
DISCUSSION
Different studies report limited English proficiency among newcomers to Canada, including Chinese populations25. Such deficiencies may affect linguistic isolation and lack of access to needed health services that promote smoking cessation5,9,13,26. Furthermore, cultural norms that normally promote smoking behaviors in Chinese communities may lead to excess smoking habit in this community, specifically among males, due to social pressures. The high smoking rates among Chinese males, especially among recent immigrants, is reported by other studies, whereas women have very low smoking prevalence rates27,28. Different studies have reported that such cultural norms and language issues may prevent smokers from Chinese communities to participate and succeed in smoking cessation programs that are mainly developed in English, with no attention to their cultural beliefs and practices29. Therefore, although the services are available for this community group, they are not accessible or acceptable due to culturally unfamiliar cessation programs14,30.
Our study examined the outcomes on two behavioral and two perception-related dependent variables, as reported by other research too30,31. Towards the behavioral variables, the results of the study showed that presenting participants with educational materials relevant to their cultural norms and in their preferred language resulted in significant decreases over time in self-reported cigarettes smoked per day and measured CO levels, as reported also by Wu et al.14. However, given that no significant interactions or main effects were observed concerning the study condition (counseling vs non-counseling), we cannot confidently claim that the counseling intervention offered any significant improvement over the educational materials alone, towards reducing smoking behaviors. However, it should be noted that this study provided accessibility to smoking cessation education to both counseling and non-counseling groups, for some of whom it was a first time to attend such a culturally and linguistically appropriate smoking cessation program30. We believe that, by being part of this study, the participants had a better understanding of the harms and benefits of smoking and, therefore, participation may have already affected smoking reduction or cessation among participants, regardless of their study group orientation. Overall, the results related to the perception-related dependent variables of self-rated importance of quitting and confidence in quitting do lend some evidence towards the efficacy of the counseling intervention. A similar finding was reported by Lee et al.32. When rating the importance of quitting over time, the Chine-sespeaking participants benefitted more than the English-speaking participants from the counseling intervention, showing a high average increase in ratings from the beginning to end of the study. Towards the ratings of confidence in quitting over time, both the Chinese- and English-speaking participants in the counseling group increased their confidence in quitting over time relative to the non-counseling group participants, on average, albeit only slightly.
Our intervention was based on relevant theoretical concepts and social support constructs33, and was delivered by health professionals and counselors from the target communities. Evidence for the effectiveness of the intervention effect was recorded by participants’ self-reported cessation or smoking reduction, which was confirmed by their exhaled carbon monoxide level. In all analyses, quit rates among the counseling group were almost double those of the non-counseling group.
Strengths and limitations
The present study includes several limitations. First, the sample size is somewhat small relative to the statistical analyses conducted here, leading to large variability and potentially underpowered hypothesis tests. Moreover, where significant findings were observed, effect sizes tended to be small, suggesting that the practical significance of our findings may be smaller than the statistical significance would suggest at first glance. Despite this limitation, the findings may warrant the feasibility of conducting a larger study to check the efficacy and effectiveness of culturally and linguistically sensitive smoking cessation in ethno-cultural communities, including Chinese-speaking smokers. In addition, participants were assigned into a group of their choice, which could influence the outcomes between the counseling and non-counseling group and bias results. However, several methodological and theoretical strengths of the study should be mentioned. This study aimed to facilitate access to trustful and practical information and quit smoking approach, by inclusion of health professionals from the target culture/language groups to provide consultations and education, which is a novel approach to help minority community to quit smoking. Additionally, the framework we applied to recruit participants from the community, as well as collect and integrate their culturally relevant smoking cessation insights, may be applicable to other ethnic minority populations, as it would be also with the linguistically and culturally appropriate educational materials that we developed in this study.
CONCLUSIONS
The primary aim of our study was to help participants cut down or quit smoking over an 8-month intervention period by applying a combination of pharmacotherapy (NRT), educational intervention, and behavioral counseling. To accomplish this goal, we developed the smoking cessation protocol, study measurement questionnaire, as well as educational and consultation materials with the direct involvement of the community members and health professionals. We also involved supportive family members in the intervention and incorporated risk perception and behavioral modification concepts into our intervention, which were crucial elements for the success of our smoking cessation program34. The results of our intervention show a significant effect on importance ratings depending on the language group, and a significant increase in confidence ratings overall. We consider this a pilot study and the results will be applied as a basis for a large-scale intervention for Chinese Mandarin and Cantonese speaking groups.