INTRODUCTION
Although smoking has been recognized as the most preventable cause of death worldwide1 and its prevalence in many countries has recently declined2, it still constitutes a major public health threat. In Europe the proportion of daily smokers in 2014 was 18.4% of the general population (aged ≥15 years), ranging from 8.7% in Sweden to 27.0% in Greece and 27.3% in Bulgaria2. Among women, the proportion was 15.1%, ranging from 8.3% in Romania to 21.3% in Greece and 22.0% in Austria2.
Numerous studies have demonstrated that prenatal smoking or exposure to smoke during pregnancy is associated with an increased risk of small-for-gestational-age infants and preterm delivery3-6, stillbirth4,7, complications such as placental abruption and premature rupture of membranes4, Sudden Infant Death Syndrome8,9 as well as several congenital malformations10,11. In addition, maternal smoking has been shown to be one of the most avoidable causes related to future health problems of childhood such as onset of childhood asthma12, neurological disorders13, childhood overweight and obesity14 and increased total mortality in future adult life15. Finally, it is speculated that it may be related to behavioral problems and cognitive delays6,16,17.
Despite the well-established negative effects of tobacco on the fetus and child, the prevalence of smoking during pregnancy, albeit declining, still remains high18-25. In Greece, the total number of births was 88553 in 201726. In two different studies published in 2010 and 2016, the prevalence of maternal smoking during pregnancy was reported at 17% and 26.3%, respectively27,28. Several factors, such as marital status, parity, educational level, living with relatives who smoked, the smoking status of partner, the frequency of smoking and alcohol abuse have been identified to be associated with cessation of smoking during pregnancy27-30.
However, smoking in pregnancy is a dynamic social phenomenon, with a prevalence changing overtime. The present study aims to determine the prevalence of smoking among pregnant women visiting the largest maternity hospital in the city of Athens, Greece, and to investigate the risk factors affecting maternal smoking during pregnancy in this population. Recording updated data with regard to the present status of this major public health problem and providing a potential feedback for healthcare authorities designing anti-smoking policies is warranted.
METHODS
Study design and population
This is a single-center, prospective, observational cohort study conducted at the Cardiology Department of a large maternity health center in Athens, Greece, between September 2016 and August 2017. The study was conducted in the cardiology department since maternal smoking in pregnancy represents a major risk factor for cardiovascular mortality and morbidity, and due to the fact that all women about to give birth in our hospital should, by the hospital’s protocol, have at least one regular cardiology assessment. In all, 1744 pregnant women visited consecutively the outpatient Cardiology Department during that period and 1700 were recruited in the study. In addition to the relatively large size of the population sample, women with various educational, social and economic levels were admitted in the study. Therefore, our population may be considered as representative with regard to the smoking status of pregnant women in Greece. All participants were residents of Athens. Participants were recruited if gestational age was ≥28 weeks, however, 64 women (3.8%) who had a gestational age of ≤27 weeks were also included in our analysis. Women who agreed to participate in the study, after giving oral informed consent, were provided with a questionnaire by the nurses, midwives or doctors of our department. All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments, and have been approved by the local Ethics Committee of our Hospital. Participants provided oral informed consent prior to enrolment in the study. In addition, they were informed by the nurses and midwives of our team about the negative consequences of smoking in pregnancy both verbally and by smoking cessation leaflets. All personal data stored in electronic and hard-copy forms were pseudonymized.
Collected data included maternal age, week of pregnancy, parity, smoking habits before and during pregnancy, absolute number of cigarettes/day both before and during pregnancy, level of education in the case that the future mother was a smoker, presence of dyslipidemia, chronic arterial hypertension and diabetes mellitus, presence of arterial hypertension and diabetes mellitus of pregnancy, and smoking status of the partner.
The prevalence of smoking in pregnancy was determined and different sociodemographic factors associated with cessation of smoking during pregnancy were identified.
Definitions
In the present study, women were classified either as non-smokers or smokers (defined as those who smoked ≥1 cigarettes/day at the time they become aware of the pregnancy). The latter were further classified as active smokers if they continued to smoke during pregnancy, even occasionally, and quitters if they had completely stopped smoking. Furthermore, women who had previous pregnancies that reached a viable gestational age (including live births and stillbirths) were defined as multipara whereas women who did not have such pregnancies previously were classified as primipara. Moreover, high educational level was considered when women had university or other higher than 12 years of school education. In this study, educational level was recorded only for smokers. In the case that a partner was present, the smoking status was classified as smoker if at least 1 cigarette/day was consumed or non-smoker if the partner was not smoking or had completely quit smoking after becoming aware of the woman’s pregnancy. Women who were single were excluded from partners’ smoking status calculations. In the case that the pregnant woman was an active smoker, we also obtained the absolute number of the cigarettes/day both before and during pregnancy in order to identify whether the burden of smoking was: not reduced (i.e. no change in the number of cigarettes/day), mildly reduced (<50%), moderately reduced (51–80%) or significantly reduced (>81%).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation, while categorical variables are presented as absolute or relative frequencies. For continuous variables, the assumption of normality was tested using the Kolmogorov-Smirnov criterion and with visual inspection of the distribution histograms. Comparisons of continuous variables (age) between smokers and non-smokers was performed using Student’s t-test for unpaired measures. Pearson’s chi-squared test was used to investigate associations among categorical variables (for example smoking status according to educational level or the smoking status of the partner). Exact p<0.05 were considered statistically significant. Data analysis was performed with SPSS software, version 18.0 (Chicago, IL).
RESULTS
Mean age was 31.2±5.5 years (range: 15–49), participants were assessed at 36±5 weeks of pregnancy (median: 37 weeks, range: 6–41) and had 1.7±0.8 number of pregnancies. Eleven women were assessed between the 11th and 20th week of pregnancy, and 6 had a gestational age of ≤10 weeks. Demographic data and co-morbidities are presented in Table 1.
Table 1
Sociodemographic data and co-morbidities of participants in the HELENA study in relation to their smoking status in pregnancy
| Characteristics | Total number (N=1700) n (%) | Non-smokers (N=996; 58.6%) n (%) | Smokers (N=704; 41.4% ) n (%) | p a |
|---|---|---|---|---|
| Age (years), Mean±SD | 31.2±5.5 | 31.3±5.3 | 31.1±5.7 | 0.68 |
| Pre-existing DM | 14 (0.8) | 8 (0.8) | 6 (0.9) | |
| DM of pregnancy | 90 (5.3) | 53 (5.3) | 37 (5.3) | |
| Pre-existing (chronic) AH | 6 (0.4) | 2 (0.2) | 4 (0.6) | |
| Gestational AH/ Preeclampsia | 94 (5.5) | 41 (4.1) | 53 (7.5) | |
| Dyslipidaemia | 19 (1.1) | 11 (1.1) | 8 (1.1) | |
| Age group (years) | ||||
| ≤20 | 45 (2.6) | 17 (1.7) | 28 (4.0) | |
| 21–30 | 702 (41.3) | 411 (41.2) | 291 (41.3) | |
| 31–40 | 905 (53.2) | 539 (54.1) | 366 (52.0) | |
| ≥41 | 48 (2.8) | 29 (2.9) | 19 (2.7) | |
| Parity (n=1700) | 0.003 | |||
| Primipara | 811 (47.7) | 446 (44.8) | 365 (51.8) | |
| Multipara | 889 (52.3) | 550 (55.2) | 339 (48.2) | |
| Partner’s smoking status (n=1513)* | <0.001 | |||
| Smoker | 463 (30.6) | 167 (16.9) | 296 (56.4) | |
| Non-smoker | 1050 (69.4) | 821 (83.1) | 229 (43.6) | |
| Educational level (n=704)** | ||||
| High | 180 (25.6) | n/a*** | 180 (25.6) | |
| Non-high | 524 (74.4) | n/a*** | 524 (74.4) | |
Of the 1700 participants, 704 (41.4%) were smokers. Of these, 369 (52.4%) quit smoking after becoming aware of their pregnancy whereas 335 (47.6%) chose to remain active smokers during pregnancy. There were no significant age differences neither between smokers and non-smokers (p=0.68) nor between active smokers and quitters (p=0.11). The overall prevalence of smoking in pregnancy in our population was, therefore, 19.7% (Figure 1). Age group analysis is presented in Table 1. None of the 369 women who quit smoking reported to have received specialized medical advice in an organized smoking cessation counseling structure.
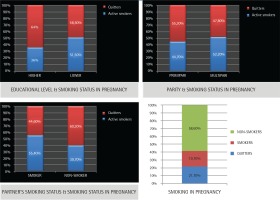
Figure 1
Prevalence of smoking and factors associated with smoking cessation during pregnancy (N=1700). (A) The effect of the maternal educational level on maternal smoking status. (B) The effect of parity on maternal smoking status. (C) The effect of partner’s smoking status on maternal smoking status. (D) Prevalence of smoking in pregnancy
Although there were no significant differences between the second, third and fourth age group, our data show that in younger women (≤20 years), the prevalence of smoking was significantly higher both before and during pregnancy (p=0.038).
Furthermore, among active smokers during pregnancy, a significant reduction was demonstrated in smoking burden as expressed by consumed cigarettes/day. Overall, reduction in cigarette consumption was recorded in 91.3% of the cases. More specifically, of 335 active smokers, 29 (8.7%) did not change their smoking habits, 49 (14.6%) reduced the cigarettes/day by <50%, 123 (36.7%) by 51–80%, and 134 (40%) by >81%.
Of the 1700 women, 52.3% were multipara (maximum 7 pregnancies). The prevalence of smoking was significantly higher in primipara women than in multipara, 45% versus 38.1%(p=0.003). However, data analysis suggests that multipara women were less likely to quit, since of the 365 primipara women who were smokers before pregnancy 56.7% quit, whereas of the 339 multipara women who smoked 47.8% quit (p=0.032).
In addition, it was demonstrated that the prevalence of smoking was higher among women whose partners were also smokers (64% vs 21.8% in women whose partners did not smoke, correlation coefficient = 0.38, p<0.001). Moreover, pregnant women who were smokers had a higher chance to quit smoking during pregnancy if the partner was a non-smoker (60.3% vs 44.6% when the partner was also a smoker, p=0.047).
Finally, in the present study, high educational level was associated with quitting smoking in pregnancy, since 64% of smokers who had higher education quit smoking compared to 48.5% of those who received ≤12 years of school education (p=0.044).
Data regarding parity, partner’s smoking status and educational level are presented in Table 2 and Figure 1.
Table 2
Sociodemographic data and co-morbidities of participants in the HELENA study who smoked before pregnancy in relation to smoking cessation during pregnancy
| Characteristics | Total number (N=1700) n (%) | Non-smokers (N=996; 58.6%) n (%) | Smokers (N=704; 41.4%) n (%) | p a |
|---|---|---|---|---|
| Age (years), Mean±SD | 31.1±5.7 | 31.4±5.2 | 30.7±6.2 | 0.11 |
| Pre-existing DM | 6 (0.9) | 4 (1.1) | 2 (0.6) | |
| DM of pregnancy | 37 (5.3) | 16 (4.3) | 21 (6.3) | |
| Pre-existing (chronic) AH | 4 (0.6) | 1 (0.27) | 3 (0.9) | |
| Gestational AH/ preeclampsia | 53 (7.5) | 22 (6.0) | 31 (9.3) | |
| Dyslipidaemia | 8 (1.1) | 4 (1.1) | 4 (1.2) | |
| Age group (years) | ||||
| ≤20 | 28 (4.0) | 9 (2.4) | 19 (5.67) | |
| 21–30 | 291 (41.3) | 155 (42) | 136 (40.6) | |
| 31–40 | 366 (52.0) | 196 (53.1) | 170 (50.1) | |
| ≥41 | 19 (2.7) | 9 (2.4) | 10 (3.0) | |
| Parity (n=704) | 0.032 | |||
| Primipara | 365 (51.8) | 207 (56.1) | 158 (47.2) | |
| Multipara | 339 (48.2) | 162 (43.9) | 177 (52.8) | |
| Partner’s smoking status (n=525)* | 0.047 | |||
| Smoker | 296 (56.4) | 132 (48.9) | 164 (64.3) | |
| Non-smoker | 229 (43.6) | 138 (51.1) | 91 (35.7) | |
| Educational level (n=704)** | 0.044 | |||
| High | 180 (25.6) | 115 (31.2) | 65 (19.4) | |
| Non-high | 524 (74.4) | 254 (68.8) | 270 (80.6) | |
DISCUSSION
This study aimed to determine the prevalence and predisposing factors of smoking among pregnant women. Participants had a mean age of 31.2 years, consistent with previously reported maternal age patterns in Greece31. Our data revealed a high prevalence of 19.7% of women who continued smoking despite the fact that they were pregnant, which remains unchanged in the last years27,28. On the other hand, 52.4% of smokers quit after becoming aware of the pregnancy. Another finding was that women who remained active smokers during pregnancy significantly reduced the number of cigarettes consumed daily.
These findings are consistent with previous research among pregnant women in Greece. A prospective mother–child cohort (n=1291, mean age: 29 years), that assessed women at week 12 of gestation27 and a more recent cross-sectional survey (n=300, mean age: 33.76 years), assessing women in the first, second and third trimesters of pregnancy28, revealed a prevalence of smoking during pregnancy of 17% and 26.3%, respectively.
In the current study, we recruited women living in a large city, in contrast to a previous study where 23% of the participants originated from rural areas27. Differences in smoking prevalence (e.g. 17% vs 19.7%) may partly be explained by this difference in study design, as living in rural areas is associated with lower smoking rates, that do not change during pregnancy27,32.
In contrast to our findings, data from several Western European countries, Australia and the USA demonstrate significantly lower prevalence of smoking during pregnancy and a steady decrease in maternal smoking rates in the last years18,19,22-24. Nevertheless, smoking in pregnancy still remains a major public health issue, with a significant heterogeneity among different geographical areas20-23,25. In a recent systematic review and meta-analysis, the global prevalence of smoking during pregnancy was estimated to be 1.7%, with the highest prevalence recorded in the European Region (8.1%). Greece is included in the subgroup of countries with a prevalence of 15.1–20.0%33,34. Additionally, in another study from Germany, more than half of all smokers did not quit smoking completely during pregnancy35.
A particularly worrying finding of the present study was the high prevalence of smoking demonstrated among younger pregnant women. In addition, younger women were less likely to discontinue smoking during pregnancy (32.1% vs 52.4% in the overall study population). These results were in line with recent data indicating that smoking rates remain high among younger pregnant women and teenagers while the prevalence of maternal smoking decreases with age22-24,36. These findings may be attributed to the advanced marketing methods used by the tobacco industry for targeting this population, and also to the psychological, biological and socioeconomic changes occurring at adolescence leading young pregnant women in adopting a high-risk life-style.
In the present work, similar to other studies, we also found that the prevalence of smoking was significantly higher in women whose partners were also smokers26,37-39. Moreover, the presence of a partner who does not smoke or quits smoking during pregnancy increased the probability of the pregnant woman quitting smoking. Furthermore, in agreement with previous research, our data suggest that primipara women and women with a higher educational level are more likely to quit smoking during pregnancy22,27,28,30,33,36,40,41.
These findings suggest that maternity units should develop specialized smoking cessation counseling structures in order to educate pregnant women, their partners and close relatives on the risks of both active and passive smoking for the fetal, infant and mother’s health. Secondly, the role of smoking cessation clinics should be improved and offered to pregnant women after referral from the counseling services. Thirdly, women of reproductive age, especially teenagers and young adults, should be educated about the potential adverse effects of tobacco by campaign programs, using mass media, social media and online courses. Moreover, a strict implementation of the existing laws, prohibiting smoking in most public places should be adopted. This strategy was proved to be effective in establishing smoke-free environments in public and work places and in reducing maternal smoking in pregnancy42. Finally, restricting exposure to tobacco industry targeting, such as banning tobacco advertisement should be introduced.
Strengths and limitations
The present study has the following strengths. First, to our knowledge, the current study is the largest of its kind in Greece, and has sufficient power to draw conclusions about the extent of the problem. Moreover, it provides useful up-to-date epidemiological data that enrich international literature, indicates that the strategies pursued so far were not effective and highlights the necessity for improved public health policies for tackling this problem.
However, this study also has several limitations. First, despite the fact that 96.2% of the recruited women had a gestational age ≥28 weeks, a group of 64 women at ≤27 weeks of pregnancy was also included in data analysis. Although this group is small it could influence the proportion of smokers and quitters of the study population. Estimates such as interruption or declining of smoking consumption during pregnancy, are highly dependent on the gestational age of recruitment, which differs largely among the included women in the present study. Second, due to the fact that miscarriage before the 20th week of gestation is a common adverse outcome due to smoking, a number of smokers might have been missed and the actual proportion of smokers in this study might have been affected, since, as we already mentioned, most subjects were recruited after the 28th week of pregnancy. Third, data regarding smoking are based on self-reporting information and therefore smoking status during pregnancy may be underreported. Previous studies have also revealed a trend towards underreporting smoker status. Fourth, partner’s smoking status may, similarly, be underreported. In addition, this information was not directly recorded from the partner, but was provided by the pregnant women. Moreover, the subgroup of non-smoker partners is heterogeneous, consisting of those who quit smoking and those being non-smokers before pregnancy. Fifth, some important parameters, such as education level of non-smoker women, important risk factors that affect the maternal smoking status, such as mental disorders and level of nicotine addiction, partner’s data (e.g. age, education) and information about passive smoking were not recorded. These data could have provided a more accurate estimate of the characteristics of maternal smoking in pregnancy. Furthermore, data regarding the use of e-cigarettes and other electronic nicotine delivery systems were not recorded. However, e-cigarette vapor or aerosol may contain several harmful substances and, in addition, chemical compounds vary between brands. Therefore, most probably, these products are not safe to use during pregnancy. Finally, the characteristics of our study population may not fully correspond to those of the general population with regard to the income and educational level. Moreover, in our study we included women who lived in the city of Athens, however, women living in rural areas may manifest different behavior regarding their smoking habits in pregnancy. A study recruiting women from different parts of the country, followed up in multiple maternity centers would probably be more representative.
CONCLUSIONS
We demonstrated that the prevalence of smoking during pregnancy still remains at unacceptably high levels. Important factors associated with cessation of smoking during pregnancy were the educational level, parity and smoking status of the pregnant woman’s partner. Public health authorities should enhance efforts to reduce maternal smoking through educating pregnant women, their partners and relatives as well as through sustained and diverse anti-smoking and tobacco-control activities.


