INTRODUCTION
Smoking accounts for an estimated 6 million deaths every year globally. By 2030, the mortality rate is expected to increase to approximately 8 million deaths annually1-3. According to the 2016 National Health Interview Survey, up to 15.5% of adults in the US smoke cigarettes, an improvement from 20.9% in 20054. The success rate of smoking cessation is within the range 5–7.4%5-7. Evidenced-based methods are less frequently used than non-evidence-based methods8, yet studies have shown that treatment with pharmacotherapy and counseling support, either individually or when combined together, increase the likelihood of success by greater than 10%9,10.
There is considerable variability among people who smoke, in terms of smoking cessation methods used and successful quitting11,12. In the 2010 National Health Interview Survey, low income and non-Hispanic Blacks indicated a higher interest in smoking cessation than non-Hispanic Whites but had lower rates of success13,14. In a separate study, Hispanics were half as likely to seek assistance with tobacco cessation compared to Whites, and heavy smokers were more likely to seek assistance compared to light smokers11. Studies have shown inconsistencies in the association between level of nicotine dependence and successful quitting12,15, and inconsistencies in the association of ENDS use and successful quitting12,16.
Gaps exist in the understanding of different subgroups of tobacco cigarette users’ willingness-to-try tobacco cessation methods including counseling and pharmaceutical products17. Identifying effective strategies for tobacco cessation, integrated with patients’ preferences, especially in a sociodemographically diverse setting, is beneficial and may lead to a reduction in tobacco-related morbidity and mortality18. The current study examines a convenience sample of US adult tobacco cigarette users’ self-report of their willingness-to-try various forms of evidence-based and non-evidence-based cessation methods. Our study investigates whether differences in participants’ preferences of tobacco cessation methods is associated with sociodemographic and tobacco use factors.
METHODS
Design
We conducted a cross-sectional online survey of various tobacco cessation methods. The study included a pre-test phase using an academic email system. Twelve individuals participated in the pretesting of the survey between 9 and 14 May 2016. We revised and simplified the language of the survey based on feedback from the pretest phase. To improve the clarity of the survey, we carried out a second round of testing with 75 participants who were recruited from a survey panel via Research Now, a market research group, between 15 and 16 August 2016. After this round of testing, we revised the survey language again and fielded the final version of the survey between 26 and 31 August 2016. Participants from the Research Now panel were compensated at the marketing group’s rates at the time. The UNC Chapel Hill School of Medicine Institutional Review Board approved this study.
Sample
The team enlisted and enrolled 900 participants, aged 18 years and older, who were members of an online survey panel of the Research Now market research group. The current analysis was limited to 562 participants who reported current tobacco cigarette use—defined as tobacco cigarette use in the past 30 days. Participants who reported ENDS use within the last 30 days in addition to tobacco cigarettes were also included in the study and were classified as dual users. All participants had to live in the United States and able to complete an online survey in English. Research Now does not provide data on how many people receive the initial invitation to participate in a study, thus we cannot report the response rate.
Measures
Data on sociodemographic characteristics collected included questions about race, education level and yearly household income. The survey also collected details about each participant’s tobacco cigarette use characteristics including number of cigarettes per day, time to first smoke after waking, and past attempts to quit. For past quit attempts, participants were asked if they have ever tried to quit smoking tobacco cigarettes. They were not asked which method they used in the past or when they attempted to quit. The heaviness of smoking index (HSI), which estimates the level of nicotine dependence as mild, moderate or high based on the number of cigarettes smoked per day and time to first smoke after waking was calculated for each participant19.
Age was categorized into the age groups: 18–34, 35–64 and ≥65 years. Some sociodemographic variables were dichotomized. Race was collapsed into non-White and White but was not further classified by ethnicity due to the low number of Hispanic participants. Education was classified as ≤high school degree/GED and ≥some college. Income was classified as <$30000 and ≥$30000. HSI was further dichotomized into high or moderate/low while quit attempts in the past year and ENDS use were categorized as yes or no. Positive responses for the use of tobacco cessation methods, i.e. ‘will definitely use’ and ‘likely to try’, were categorized as willingness-to-try for the analysis.
Outcome measures
Participants were asked to rate their willingness-to-try different forms of evidence-based and non-evidenced-based tobacco cessation methods. Response options included: ‘would definitely use’, ‘likely to try’, ‘unlikely to try’, and ‘would definitely not try’. Evidence-based methods listed were medications including nicotine containing products, Wellbutrin/Zyban and Chantix, and different forms of counseling support including individual counseling, support group or class, telephone quitline, online program, texting program, and any counseling. Non-evidenced-based methods included forms of complementary and alternative therapy, other tobacco or nicotine delivery systems, and quitting without any assistance. Participants were not informed which methods are evidence-based or non-evidence-based.
Analysis
Bivariate associations between ENDS use (yes/no) and baseline characteristics (i.e. sociodemographic characteristics and tobacco use characteristics) were examined using t-tests for normally distributed continuous variables, Wilcoxon-Mann-Whitney tests for non-parametric continuous variables, and chi-squared tests for categorical variables. Unadjusted and adjusted effects were estimated for willingness-to-try cessation methods using logistic regression. The cessation methods of focus were recommended methods of quitting in the form of any medication, any counseling, any evidence-based cessation method, and quitting ‘cold-turkey’. ‘Cold-turkey’ was chosen as the independent quitting method because it is the most common method used for quit attempts. Purposeful selection method was used20 to determine variables to include in adjusted models, which involved an iterative process of examining all covariates as potential significant predictors or confounders. In the iterative process, covariates were removed from the model if they were non-significant at α=0.1 and not a confounder (i.e. did not result in a parameter estimate change greater than 15%). The final model included only significant covariates and confounders. Data were analyzed using SAS version 9.4 (SAS Institute, Inc.) with a two-tailed significance level (p<0.05). Risk ratios are reported rather than odds ratios because the outcome events are relatively common (incidence of more than 10%) and thus risk ratios offer more appropriate approximations21.
RESULTS
From the larger sample of 900 participants who completed the survey, 562 were tobacco cigarette or dual users. Mean age was 47 years. Most participants were White (82%), 47% were female and 76% had college education or higher. Approximately 24% of participants had an annual household income of less than $30000. Of this sample, 88% reported smoking less than 20 cigarettes per day, 14% reported less than 5 minutes to first smoke after waking and 6.2% had a high HSI score. Eighty-three per cent reported attempting to quit smoking in the past year and almost half (48%) were dual users (Table 1).
Table 1
Sociodemographic characteristics (N=562)
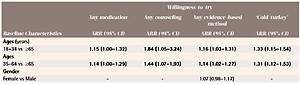
Adjusted logistic regression analysis showed that adults in the age groups 18–34 or 35–64 years were more likely to report willingness-to-try any medication, any counseling, any evidence based method and quit ‘cold-turkey’ compared to adults aged ≥65 years (Table 2). Non-White participants were more likely to report willingness-to-try any counseling method (RR=1.32, 95% CI: 1.14–1.52) compared to Whites, while participants with a high school education or less were less likely to report willingness-to-try any counseling method compared to those with a college education or higher (RR=0.78, 95% CI: 0.64–0.95). Participants with an annual income of less than $30000 were less likely to report willingness-to-try any medication (RR=0.84, 95% CI: 0.73–0.98) and any counseling (RR=0.82, 95% CI: 0.67–0.99) compared to participants with higher annual income.
Table 2
Association between baseline characteristics and willingness-to-try cessation methods among tobacco cigarette users (N=562)
Participants with a high HSI score were more likely to report willingness-to-try any medication, any counseling and any evidenced-based method (RR=1.07, 95% CI: 1.04–1.10) and less likely to report willingness-to-try ‘cold-turkey’ (RR=0.90, 95% CI: 0.87–0.94). Those who had attempted to quit in the past were also more likely to report willingness-to-try any medication, any counseling and any evidenced-based method (RR=1.31, 95% CI: 1.10–1.56) compared to those with no history of quit attempts. Although dual users were more likely to report willingness-to-try any counseling and any evidenced-based method compared to tobacco cigarette only users, these associations lost statistical significance after adjusting for other variables in the final model (Table 2).
Table 3 represents a breakdown of comparison of willingness-to-try different tobacco cessation methods among tobacco cigarette-only users and dual users. Dual users were more likely to report a willingness-to-try Wellbutrin compared to tobacco-only users with similar non-significant trends for other medications (41% vs 30%; p=0.005). Dual users were significantly more likely to report willingness-to-try any type of counseling support listed, except for individual counseling, which did not reach statistical significance. Overall, dual users were more likely to report a willingness-to-try any evidence-based method compared to tobacco cigarette only users (82% vs 73%; p=0.01). Dual users were also more likely to report willingness-to-try non-evidenced-based methods including different forms of complementary and alternative methods and other tobacco or nicotine delivery systems.
Table 3
Willingness-to-try tobacco cessation methods, n (%)
DISCUSSION
The current study explores a convenience sample of tobacco users’ willingness-to-try different tobacco cessation methods by sociodemographics and level of nicotine dependence. Our findings reveal that preferences for tobacco cessation methods exist based on race/ethnicity, level of income, education and severity of nicotine dependence. While non-White participants were significantly more likely to report willingness-to-try counseling over other cessation methods, those with lower education level were less likely to report willingness-to-try counseling and those with an annual household income of less than $30000 were less likely to report willingness-to-try any medication. Participants with a higher HSI, i.e. higher tobacco dependency, were more likely to report willingness-to-try any evidence-based cessation method over non-evidence-based methods. The data also indicate that dual users were more likely to report willingness-to-try any evidenced-based method compared to tobacco cigarette-only users.
Our results have implications for public health practice, primary care clinician counseling services and for future research. We found that young and middle-aged adults were more likely to report willingness-to-try any medication, any counseling, any evidence-based method and quit ‘cold-turkey’ compared to adults aged ≥65 years. This is inconsistent with some findings in the literature. One study showed that older adults are more likely to use counseling than young and middle-aged adults, but are less likely to be prescribed nicotine replacement therapy22, which may explain the low likelihood of willingness-to-try any medication found in our study. Older adults may also be concerned about side effects of nicotine replacement therapy and other smoking cessation medications23. Another study found that both the old and young adults are less likely to use pharmacotherapy and less likely to use evidence-based methods but more likely to use substitutes such as ENDS products. Young adults, however, are less likely to use evidence-based methods compared to old adults, which may be due to the high level of confidence they have that they can quit without assistance or concerns about the effectiveness of evidence-based methods24.
Our finding that non-White participants had a higher likelihood to report willingness-to-try counseling compared to Whites is similar to previous studies that showed a higher utilization of quitlines and telephone counseling by non-Whites compared to White tobacco users in studies that assessed variations in quitline reach by ethnicity and race25,26. This preference for counseling over other methods may arise from lack of knowledge or awareness about pharmacological therapies, their perceived costs, harms or their effectiveness, leading to a perceived preference for counseling. Some studies have shown that, compared to White tobacco users, non-Whites are less likely to be screened for tobacco use or advised to quit by a healthcare provider27,28 and hence, may not be aware of all their options. Another study to assess ethnic minority group’s beliefs and perspectives for recommended treatment options for tobacco cessation found that many participants were not fully aware that medications are beneficial and were concerned about risks of side effects29. These concerns may have contributed to findings in the current study and may explain why non-Whites reported willingness-to-try counseling over other methods.
We found that participants with an annual income less than $30000 were less likely to report willingness-to-try any medication and counseling. This finding may be related to costs especially for low-income smokers who may be uninsured. While the daily cost of cessation medications, for example, may be similar to the cost of cigarettes, these medications tend to come in weekly or monthly supply, making it unaffordable for low-income smokers who may need to pay out-of-pocket30, especially for low-income patients31. This association has been mentioned in other studies that showed that low-income patients with chronic disease cut back on essential medications or are non-adherent due to cost32,33. Removal of the cost barrier or the offer of free treatment may increase preference and hence use of pharmacotherapy for tobacco cessation among low-income patients34. An annual household income of less than $30000 was also associated with a lower likelihood of reporting willingness-totry any counseling. Although one might expect that the lower cost of counseling makes it an attractive cessation method for low-income smokers, studies have shown the opposite35. Elements such as distrust and lack of knowledge have been cited as reasons for the low utilization of counseling among low-income smokers36,37. Other challenges such as access to healthcare settings that can also provide smoking cessation services including counseling, health issues related to depression and substance or alcohol abuse, in addition to daily challenges, may make counseling for smoking cessation less attractive to low-income smokers38.
Although we found that participants with lower levels of education were less likely to indicate a willingness-to-try any counseling, other studies have shown mixed results, indicating a positive, negative or non-significant association between low education and participation in counseling11,39-41. Our findings may be a result of the fact that people with low educational status are less likely to receive smoking cessation advice28,42 and hence may not be aware of counseling as an option.
Tobacco use characteristics seem to play a role in willingness-to-try different cessation methods. Participants with a high level of nicotine dependence were more likely to report a willingness-to-try any evidence-based method and less likely to report willingness-to-try to quit ‘cold-turkey’. This is similar to findings by Zhu et al.11 who found that heavy smokers were twice as likely to seek assistance as light smokers. In this study, the assistance involved both evidence-based and non-evidenced-based methods such as self-help materials. The fact that those with high level of nicotine dependence are less likely to quit ‘cold-turkey’ may stem from previous failed attempts to quit without assistance or concerns that the severity of their nicotine dependence may make it challenging to quit independently.
In addition, participants with a history of previous quit attempts were more likely to report willingness-to-try any evidence-based method. A similar study that assessed preferences for future quit attempts showed that a history of previous quit attempts with medications was associated with interest in pharmacotherapy for future quit attempts43. Another study showed that smokers tend to use the same cessation methods that they tried at their baseline quit attempt44. It is unclear if participants in our study reported willingness-to-try evidence-based methods based on cessation methods used in previous quit attempts.
Our study also showed that dual users were more willing to report a willingness-to-try both evidence and non-evidenced-based methods compared to tobacco cigarette-only users. The significant difference noted between the two groups suggests that dual users are willing to try any method in an attempt to stop smoking. However, after adjusting for other sociodemographic and tobacco use variables, no statistically significant difference was found. This suggests that other characteristics involved, such as their tobacco use habits, may have a stronger influence than dual-use and affect their likelihood to use certain methods over others. Furthermore, findings from various studies have shown that ENDS users are likely to attempt to quit overall45,46, and for some, ENDS use may be their cessation method of choice47.
Limitations
Limitations of this study include its cross-sectional design and restriction to those able to complete an online survey. Since the study was on volunteer participants, the findings may not be applicable to the general population. The cross-sectional nature also limits the ability to explore causality and to capture other factors that may affect responses of participants. Participants were not asked about their knowledge of smoking cessation methods and may not have been aware of all methods or their efficacy, which may have affected their report of willingness-to-try different methods. Another limitation is the reliance of self-reported information about smoking status and habit, which may not reflect true characteristics. Our findings reflect participants’ willingness-to-try different methods and may not correlate with actual choices. Responses to questions may also have been affected by participants’ recall bias. The level of nicotine dependence was measured by the heaviness of smoking index (HSI), which is a validated tool for measuring dependence on cigarette smoking. Hence, findings of this study may not be applicable to users of other combustible tobacco or non-combustible products. The association between the different sociodemographic groups and the willingness-to-try different cessation methods was limited to evidence-based methods and the most common independent quit method. ENDS and other cessation methods were not included in the analysis of sociodemographics and willingness-to-try different cessation methods. Furthermore, we were unable to analyze for differences between minority race and ethnicities due to the limited number of non-White or Hispanic individuals in our sample.
CONCLUSIONS
Despite improvement in the availability of interventions for smoking cessation, success rate is still suboptimal. To close this gap, efforts have been made to increase access to evidence-based methods of cessation but some methods remain preferred over others. Findings of this study highlight preferred methods for smoking cessation based on sociodemographics and level of nicotine dependence. The implication is that medical providers and those involved in the provision of tobacco cessation programs need to be mindful that individuals can differ in their preference for a smoking cessation method based on factors such as sociodemographics and nicotine dependence. In addition, increased education on evidenced-based tobacco cessation methods for smokers trying to quit will be beneficial. Further studies to evaluate methods actually used by former tobacco users of different sociodemographics and level of nicotine dependence will be helpful and may aid in the development of targeted therapies for patients to increase the likelihood of success in their smoking cessation efforts.