INTRODUCTION
The outbreak of the novel coronavirus disease-2019 (COVID-19) was declared a global pandemic by the WHO on 11 March 2020. Currently, Europe has become the epicenter of the pandemic, and the UK has been one of the hardest hit countries. In reaction to the pandemic, starting on 23 March 2020, the UK government implemented social distancing measures, lockdowns, and restrictions on individual movements to control the spread of the virus1. It was not until mid May that the gradual relaxation of the restrictions was introduced. During this unprecedented crisis, recent studies have highlighted the psychological and behavioral effects of COVID-19, including widespread mental disorders such as anxiety or depression2, and changes in tobacco use patterns3. Additionally, these pandemic-induced adverse psychological outcomes may increase the risk of addictive substance abuse and engaging in addictive behaviors4, further weakening the immune system and increasing vulnerability to COVID-19 infection5,6. This is particularly relevant for nicotine addiction, as smokers may rely on tobacco and nicotine as their main method to manage stress and anxiety7.
In this context, this study aims to provide epidemiological evidence of the changes in smoking behavior among British smokers in response to the COVID-19 pandemic and, more importantly, understand how demographic and psychosocial factors impact these behaviors.
METHODS
An analysis was conducted via a web-based survey using the UK arm of the international COVID-19 DATA TRACKER8, a joint study of Imperial College London and YouGov. The study is an ongoing online weekly survey during the COVID-19 pandemic. A pooled sample of 4075 respondents aged >16 years was surveyed between 27 April and 24 May 2020 after the first month of stringent lockdown measures when outdoor activities were continuously restricted. The sample was weighted and designed to be representative of the general UK population in terms of age, gender, and region.
Individuals responded to questions regarding demographics, current smoking status, changes in smoking behaviors and psychosocial characteristics in response to the COVID-19 pandemic. Smoking in this survey refers to the use of all combustible tobacco products (excluding e-cigarettes). Psychosocial variables included occupational social class (A, B, C1, C2, D, E), concern about mental health (worried or not worried), experiences of mental health problems (anxiety, stress, low mood and sleeping problems), the Patient Health Questionnaire9 severity index (normal, mild, moderate, and severe) and the 10-point Cantril Ladder scale ranking10 (suffering: 0–3, struggling: 4–6 and thriving: 7–10). In this study, we used the Patient Health Questionnaire (PHQ) as an index of the severity of mental disorders and the Cantril Ladder scale as a measurement of psychosocial wellbeing and life satisfaction.
The weighted sample characteristics and prevalence of the three smoking behavior groups (increased, unchanged or decreased smoking) were calculated. To analyze the relationship between smoking behavior change and the respondents’ psychosocial characteristics, Pearson’s χ2 (or Fisher’s exact test when appropriate) and Cramer’s V statistics were used. Adjusted residuals larger than |1.96| (α=0.05) were used to identify cells contributing to differences between groups in χ2 tests11. Furthermore, the Cochran-Armitage test for trend was used to determine whether there was a linear trend in the prevalence between different levels of psychosocial variables. An alpha level of 5% was used to indicate a statistically significant difference for all hypothesis tests.
RESULTS
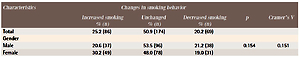
The prevalence of current smoking was 16.0% (17.4% for males and 14.7% for females) in this UK survey. Of the 486 current smokers surveyed, 329 current smokers who reported data on smoking behavior change were included in the analysis. One-quarter (25.2%, n=86) of current smokers reported smoking more than usual, with the majority being young female smokers aged 16–29 years; 50.9% (n=174) of smokers reported smoking the same amount and 20.2% (n=69) mostly young males aged 16–29 years, reported smoking less.
Table 1 presents the weighted prevalence of smoking behavior change stratified by demographic and psychosocial characteristics. The percentages of smoking behavior change did not differ by age, sex or social grade. However, there were significant differences in concerns about mental health (p<0.001), feelings of anxiety (p<0.001), stress (p<0.001) and low mood (p=0.012) during the pandemic. The differences were driven largely by respondents who reported an increase in smoking during the pandemic. More specifically, among smokers who reported worrying about their mental health, 42.3% smoked more during the pandemic, while 21.7% smoked less. The patterns were generally similar for respondents who experienced more anxiety, stress and low mood.
Table 1
Demographic and psychosocial characteristics between respondents in different smoking behavior groups, weighted (N=329)
| Characteristics | Changes in smoking behavior | ||||
|---|---|---|---|---|---|
| Increased smoking % (n) | Unchanged % (n) | Decreased smoking % (n) | p | Cramer’s V | |
| Total | 25.2 (86) | 50.9 (174) | 20.2 (69) | ||
| Gender | |||||
| Male | 20.6 (37) | 53.5 (96) | 21.2 (38) | 0.154 | 0.151 |
| Female | 30.2 (49) | 48.0 (78) | 19.0 (31) | ||
| Age (years) | |||||
| 16–29 | 33.4 (27) | 33.9 (28) | 26.2 (21) | 0.104 | 0.219 |
| 30–39 | 26.9 (17) | 51.0 (32) | 17.8 (11) | ||
| 40–49 | 23.0 (18) | 51.2 (40) | 21.0 (16) | ||
| 50–59 | 25.5 (13) | 56.9 (29) | 17.5 (9) | ||
| 60–69 | 12.6 (5) | 69.4 (29) | 15.6 (6) | ||
| ≥70 | 21.6 (6) | 61.0 (17) | 17.4 (5) | ||
| Social gradea | |||||
| A | 19.9 (6) | 46.7 (13) | 33.4 (9) | 0.175 | 0.206 |
| B | 28.2 (6) | 46.8 (9) | 25.0 (5) | ||
| C1 | 25.9 (26) | 42.8 (43) | 27.9 (28) | ||
| C2 | 31.5 (18) | 55.9 (32) | 10.9 (6) | ||
| D | 24.3 (15) | 59.6 (38) | 16.1 (10) | ||
| E | 21.3 (16) | 53.4 (39) | 13.9 (10) | ||
| Mental health | |||||
| Worried | 42.3 (39)* | 35.1 (33) | 21.7 (20) | <0.001 | 0.406 |
| Not worried | 17.3 (25) | 59.5 (86) | 20.7 (30) | ||
| Anxiety | |||||
| Less | 31.5 (5) | 28.8 (5) | 30.3 (5) | <0.001 | 0.348 |
| Same | 12.1 (15)* | 63.3 (77)* | 17.6 (21) | ||
| More | 40.2 (43)* | 36.7 (39)* | 22.4 (24) | ||
| Stress | |||||
| Less | 32.6 (10) | 41.1 (12) | 14.1 (4) | <0.001 | 0.314 |
| Same | 13.1 (14)* | 64.8 (68)* | 17.4 (18) | ||
| More | 36.9 (41) | 37.4 (41) | 24.9 (28) | ||
| Low mood | |||||
| Less | 23.7 (4) | 39.5 (7) | 36.7 (7) | 0.012 | 0.234 |
| Same | 18.9 (20) | 60.3 (65) | 16.0 (17) | ||
| More | 32.2 (38) | 41.9 (49) | 22.3 (26) | ||
| Sleep problems | |||||
| Less | 29.5 (5) | 42.2 (7) | 28.3 (5) | 0.051 | 0.199 |
| Same | 19.2 (24) | 58.5 (73) | 20.2 (25) | ||
| More | 33.8 (36) | 40.6 (43) | 19.3 (20) | ||
| PHQ | |||||
| Normal | 21.1 (29) | 56.2 (78) | 21.6 (30) | 0.018 | 0.217 |
| Mild | 16.9 (14) | 54.0 (26) | 22.8 (20) | ||
| Moderate | 36.8 (22) | 45.5 (27) | 14.1 (8) | ||
| Severe | 38.3 (20) | 38.3 (20) | 20.0 (10) | ||
| Cantril Ladder | |||||
| Thriving | 18.1 (21) | 55.2 (64) | 26.7 (31) | <0.001 | 0.257 |
| Struggle | 21.8 (43)* | 39.1 (77) | 39.1 (77)* | ||
| Suffer | 36.1 (22)* | 54.1 (33) | 9.8 (6)* | ||
* Adjusted residuals greater than |1.96|, contribute to differences between groups in χ2 or Fisher’s exact tests when p<0.05. PHQ: patient health questionnaire.
a Occupational social grade: AB – higher or intermediate managerial, administrative or professional occupation; C1 – supervisory or clerical and junior managerial, administrative or professional; C2 – skilled manual workers; D – semi-skilled and unskilled manual workers; E – state pensioners, casual and lowest grade workers, unemployed with social benefits only.
The percentages of smoking behavior change also differed according to PHQ score (p=0.018) and the Cantril Ladder ranking (p<0.001). A larger percentage of respondents who smoked more had moderate to severe PHQ index and a lower ranking on the Cantril Ladder scale, while a greater percentage of participants who smoked less reported normal to mild PHQ index and a higher ranking on the Cantril Ladder scale. Additionally, Cochran-Armitage tests for trend show that there was a statistically linear trend between the proportions of increased smoking among current smokers and the PHQ score (21.1% to 38.3%; p=0.002) as well as the rankings on the Cantril Ladder scale (18.1% to 36.1%; p=0.012).
DISCUSSION
The study findings suggest that a quarter of current UK smokers have increased their smoking during this unprecedented time, and that mental health status and psychosocial well-being were strongly associated with tobacco consumption. This phenomenon was more pronounced among those reporting deteriorated mental health and well-being. The results were in line with previous evidence reporting the relationship between smoking and depression/anxiety12.
In the present study, smokers also expressed that the pandemic had a more negative impact on their mental health. A significant linear trend between proportions of increased smoking and both the PHQ score and the ranking on the Cantril Ladder scale indicates that a worsening mental health condition and worse psychosocial well-being were linked to increased smoking. Given the worsening conditions of mental well-being, smokers are likely to increase their consumption as a coping mechanism during the pandemic7.
From the outset of the COVID-19 pandemic, paramount evidence has indicated that smoking was a risk factor for COVID-195. Studies suggest that smoking and exposure to nicotine are linked to increased risk of COVID-19 infection13 and smokers are at higher risk of having adverse outcomes after becoming infected14. However, the psychosocial impact of the pandemic with associated stress and anxiety evoked by confinement and fear of the disease could lead current smokers to increase tobacco use and former smokers to relapse15. Thus, it is essential that controlling the disease during the global pandemic requires comprehensive management and support for mental health, especially among vulnerable populations such as quarantined people and individuals with pre-existing mental conditions who are at higher risk for smoking and other addictive behaviors.
Preventing the infection is currently the best treatment available at the individual and national levels. Thus, smokers should adopt healthy coping strategies such as physical activities, meditation or yoga as a means to deal with stress and anxiety16-18. Current smokers are urged to take advantage of this opportunity to quit permanently while former smokers should maintain their quit status. Most importantly, public health authorities should take proactive measures to support the psychological well-being of the people to mitigate the impact of the pandemic19. Moreover, smoking cessation campaigns should be conducted while advising preventive measures to tackle the pandemic. Behavioral support for quitting smoking such as digital platforms, quitlines and internet programs should also be strengthened to support smokers quitting successfully during this critical time.
Limitations
Limitations of this study include that the data collection was based on online self-reported surveys, which inevitably may be at risk of misclassification and response bias. Furthermore, as this report is a preliminary investigation of smoking behavior change among current smokers during the pandemic, limited data on the frequency of smoking and other potentially related characteristics of the respondents were not taken into account. Future studies should also follow-up smoking status change among former or never smokers to investigate whether recent quitters or never smokers have relapsed or initiated smoking and to better understand the long-term effects of this pandemic on smoking behaviors.
CONCLUSIONS
Deterioration of mental health and psychosocial well-being were linked to increased smoking. The study findings emphasize the need for public health authorities to provide mental healthcare and smoking cessation support as a preventive measure to tackle the pandemic with a particular focus on vulnerable individuals who are at high risk for addictive behaviors.